Session Information
Date: Sunday, November 17, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Radiographs and MRI are the two imaging techniques often used to assess structural lesions in axial spondyloarthritis (axSpA). A high prevalence of degenerative lesions (DLs) in the spine has been reported among patients diagnosed with axSpA1 but their natural course is not well-known. Our aim was to investigate the DLs and their changes over 10 years (10Y) in patients with axSpA.
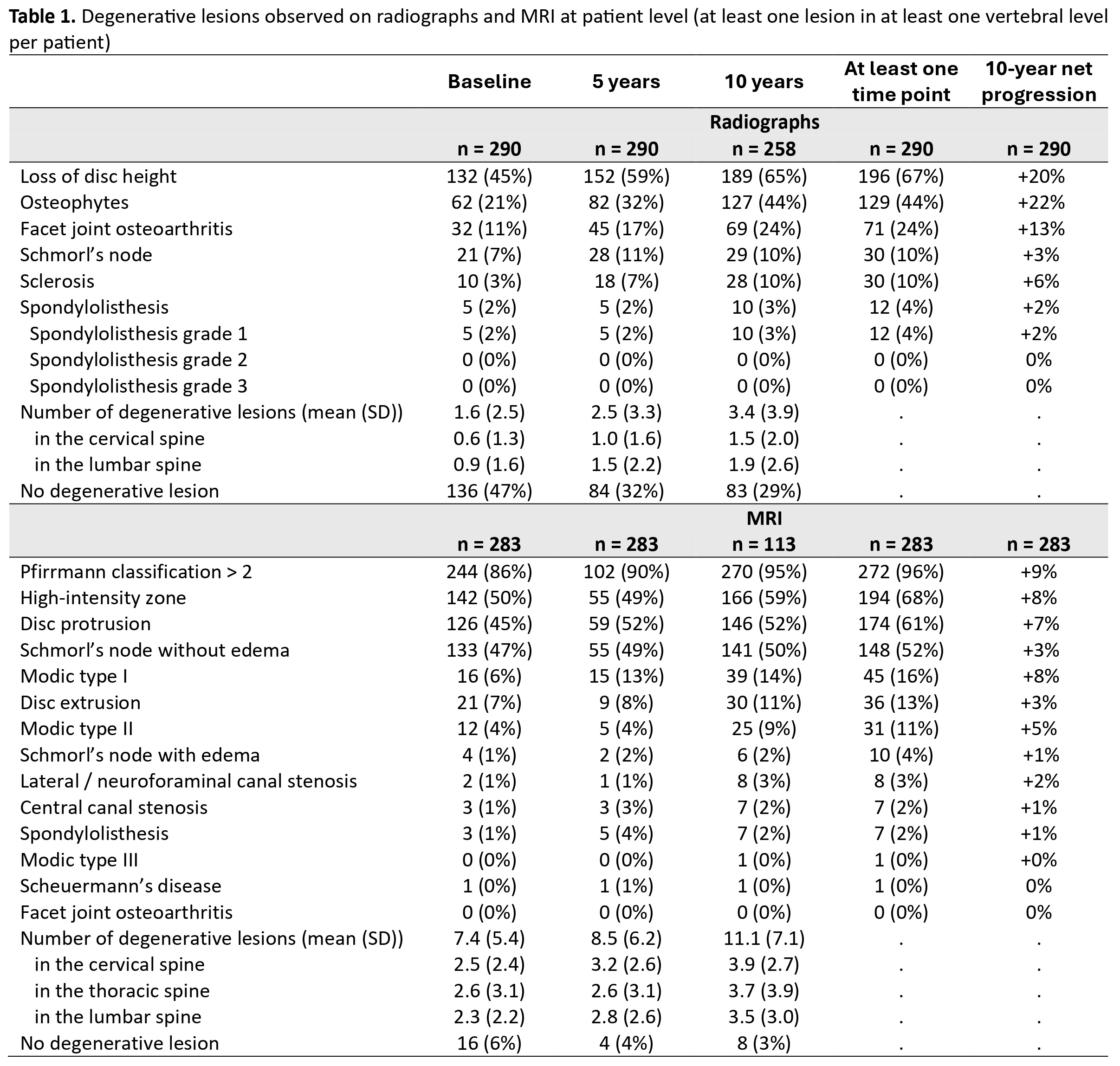
Methods: Cervical and lumbar spine radiographs and whole spine MRI at baseline, 5Y and 10Y of patients diagnosed with axSpA in the DESIR cohort were assessed for DLs by three central readers blinded to timepoint and to clinical, laboratory or any other imaging information1. Only patients with baseline and 10Y data were analyzed. The presence of each degenerative lesion was based on agreement between ≥2 out of 3 readers and an average of 3 central readers for continuous results was used (Table 1). Patient characteristics and the presence of DLs at the patient (≥1 lesion in ≥1 vertebral level) and at vertebral unit levels were reported. Net progression between 0 and 10Y was calculated by subtracting the patients that “improved” (with no specific lesion at 10Y in a patient who had ≥1 such lesion in ≥1 vertebral level at baseline) from those that “worsened” (with ≥1 specific lesion in ≥1 vertebral level at 10Y in a patient who had no such lesion at baseline) divided by the total number of patients. Finally, we compared the number of degenerative lesions at baseline and at 10Y on both imaging modalities using paired Student’s t-tests.
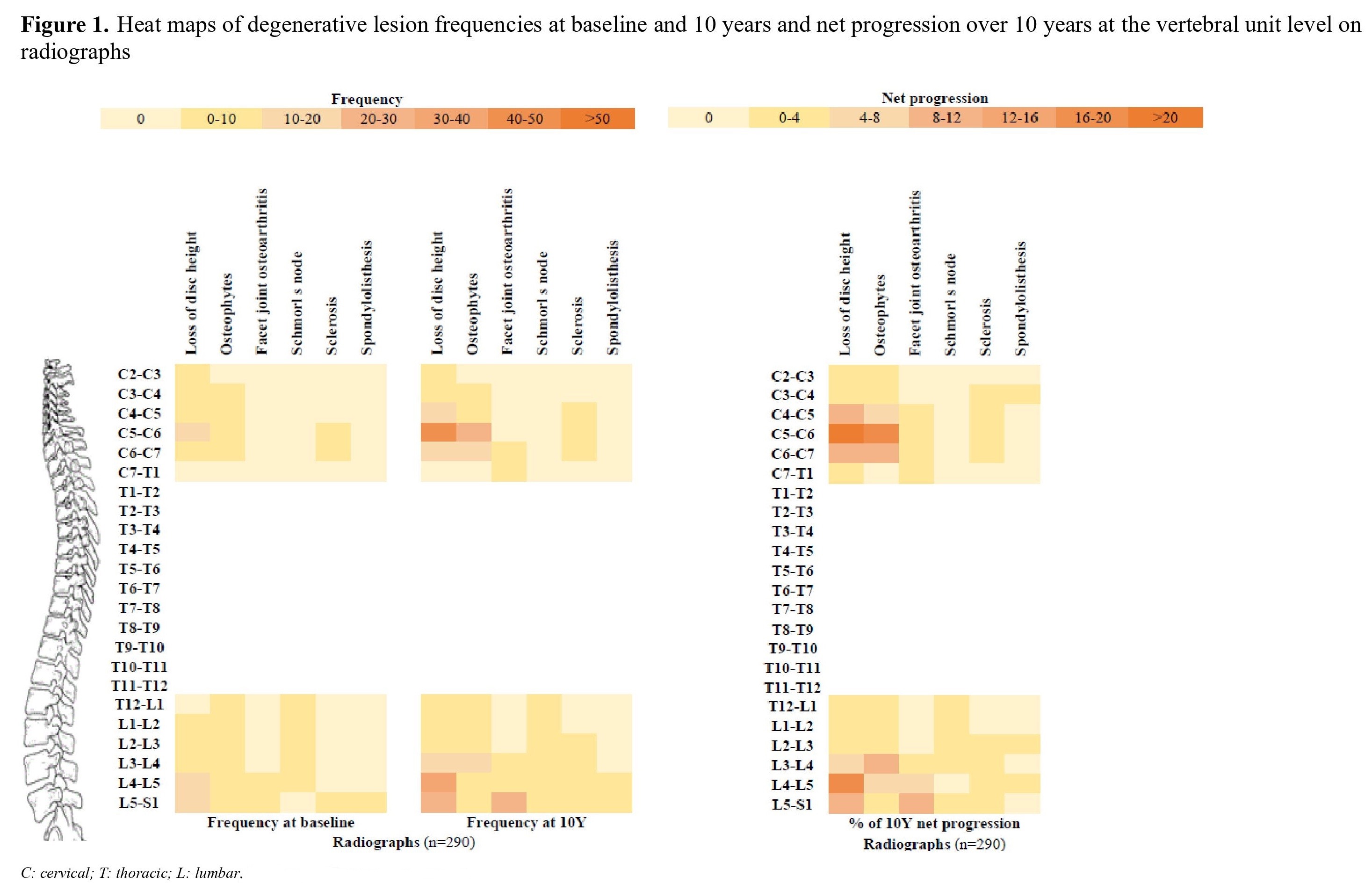
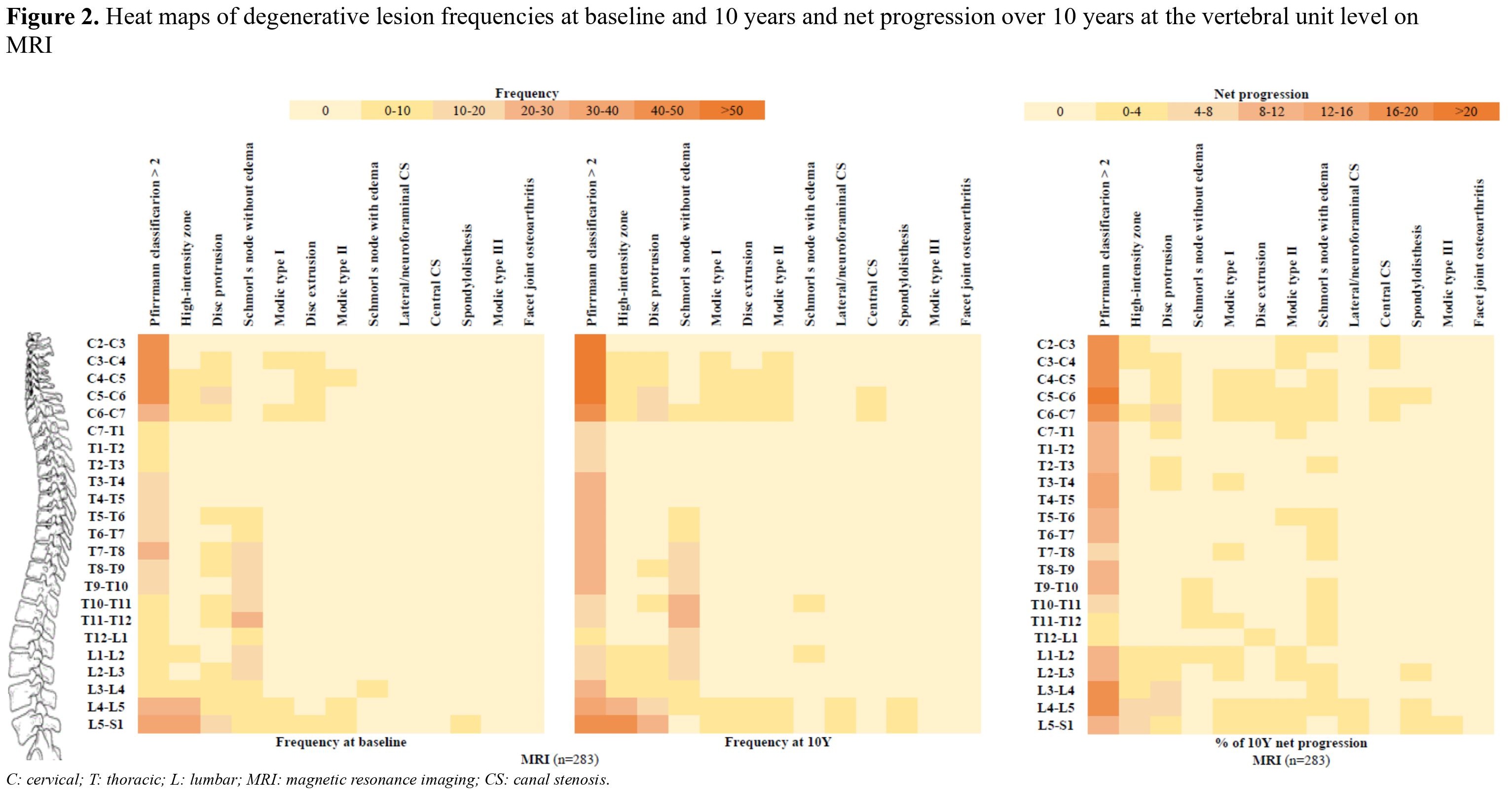
Results: Imaging was available for 291 patients (mean age [SD] 34.5 [8.6] years, 47% male). The most frequent DLs on radiographs were loss of disc height (45% at baseline, 65% at 10Y, net progression: +20%), followed by osteophytes (21% at baseline, 44% at 10Y, net progression: +22%) and facet joint osteoarthritis (11% at baseline, 24% at 10Y, net progression: +13%) (Table 1). An average of 1.6 (2.5) DLs per patient were observed on radiographs at baseline; this number increased to 3.4 (3.9) at 10Y (p-value < 0.0001). In total, 47% of patients had no degenerative lesions at baseline and 29% at 10Y. The most frequent degenerative lesions on MRI were disc degeneration (Pfirrmann classification >2: 86% at baseline, 95% at 10Y, net progression: +9%), followed by high-intensity zone (50% at baseline, 59% at 10Y, net progression: +8%), Schmorl’s node without edema (47% at baseline, 50% at 10Y, net progression: +3%) and disc protrusion (45% at baseline, 52% at 10Y, net progression: +7%) (Table 1). An average of 7.4 (5.4) DLs per patient were observed on MRI at baseline; this number increased to 11.1 (7.1) at 10Y (p-value < 0.0001). Only 6% of patients had no degenerative lesions at baseline and 3% at 10Y follow-up. The distribution of these spinal lesions is shown in the heat maps (Figures 1 and 2).
Conclusion: The prevalence of spinal DLs is high in an inception cohort of axSpA with the total number of DLs increasing over 10Y in all parts of the spine on both radiographs and MRI. Therefore, in axSpA, DLs are important to be borne in mind when interpreting imaging, particularly after several years of follow-up.
Reference: 1. de Bruin F et al. RMD Open. 2018:4(1);e000657.
To cite this abstract in AMA style:
PINA VEGAS L, van Lunteren M, Loeuille D, Morizot C, Newsum E, Ramiro S, van Gaalen F, SARAUX A, Claudepierre P, Feydy A, van der Heijde D, Reijnierse M. Natural Course of Degenerative Lesions of the Spine on Radiographs and MRI in Axial SpondyloarthritisFollowed 10 Years in the DESIR Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/natural-course-of-degenerative-lesions-of-the-spine-on-radiographs-and-mri-in-axial-spondyloarthritisfollowed-10-years-in-the-desir-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/natural-course-of-degenerative-lesions-of-the-spine-on-radiographs-and-mri-in-axial-spondyloarthritisfollowed-10-years-in-the-desir-cohort/