Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: To assess the presence of organ-specific autoimmune diseases in a cohort of patients with primary Sjögren’s Disease (SjD).
Methods:
We retrospectively reviewed the records of 328 patients who attended our tertiary reference center to assess the presence of organ-specific autoimmune diseases. We recorded the following organ-specific autoimmune diseases: gastrointestinal (primary biliary cirrhosis (PBC), autoimmune hepatitis (AH), celiac disease), hematologic (pernicious anaemia, hemolytic anemia, idiopathic thrombocytopenia purpura (PTI)) , neurologic (myasthenia gravis (MG)), dermatologic (vitiligo, alopecia areata), renal (membranous glomerulonephritis), and endocrinology (autoimmune thyroid disease (ATD) and type 1 diabetes) involvement. We also registered demographics, glandular and extraglandular features, Schirmer-1 test, non-stimulated whole salivary flow (NSWSF), serologic variables, treatment, and ESSDAI score at diagnosis. We used descriptive statistics, and performed the t-student test, the X2 test and the Mann-Whitney U- test according to the distribution of the variables. We performed a logistic regression analysis and reported OR with 95% CI. We used SPSS and considered a p value < 0.05 as significant.
Results: Most patients were female (95.7%) with a mean age of 60.5±14.7 years, and a median disease duration of 10.4 years. We observed organ-specific autoimmunity in 122 patients (31.1%). The distribution of organ-specific involvement was: autoimmune hypothyroidism (n= 56), PBC (n=28), autoimmune hepatitis (n=8), overlap PBC/autoimmune hepatitis (n=10), Graves’ disease ( n=9), PTI (n= 5), vitiligo ( n=4), celiac disease ( n= 3) , membranous glomerulonephritis (n= 2), MG (n=1) and type 1 DM ( n=1). The organ-specific disease diagnosis precede SjD in 38 patients (31.1%) , followed it in 61 patients (5%), and was concomitantly in 23 patients ( 18.8%).
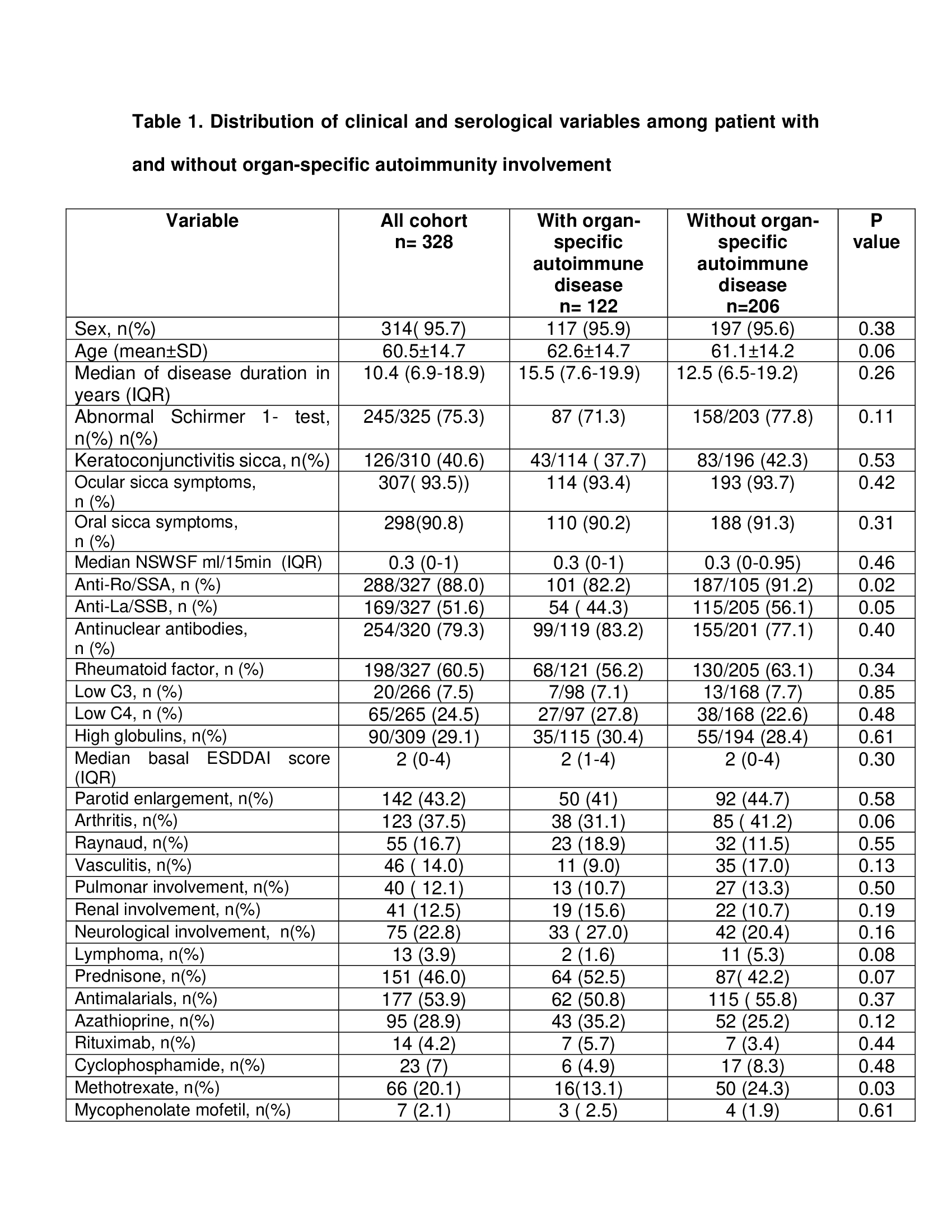
We then compared patients with (n=122) and without (n=206) specific-organ autoimmune involvement (Table 1). Both groups had similar sex, age, oral and ocular symptoms, parotid gland enlargement, Schirmer-I test, NSWSF, basal ESSDAI score and extraglandular involvement. The specific-organ autoimmune group had a lower frequency of anti-Ro/SSA (82.8% vs 91.2, p=0.02) and anti-La/SSB (44.3% vs 56.1%, p=0.05), but a similar prevalence of ANA, RF, low C3 and low C4. Regarding treatment, the groups were similar in the use of prednisone, antimalarials and immunosuppressants, with the exception of methotrexate, which was used less frequently by the organ-specific autoimmunity group (13.1% vs 24.3%, p=0.03).
In the regression analysis that included all significant variables ,and variables with a statistical tendency, the presence of anti-Ro/SSA (OR 0.47, 0.24-0.94 (95% CI), p=0.03) and the use of methotrexate (OR 0.47, 0.26-0.90 (95% CI), p=0.01) remained associated with the presence of organ-specific autoimmunity.
Conclusion: One third of patients with primary SjD had organ-specific autoimmunity, being the endocrinology involvement the most frequently seen. Organ-specific autoimmunity may precede, follow or accompany the diagnosis of SjD.
To cite this abstract in AMA style:
Hernández-Molina G, Garcia-Torralba A. Organ-Specific Autoimmune Involvement in Primary Sjögren’s Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/organ-specific-autoimmune-involvement-in-primary-sjogrens-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/organ-specific-autoimmune-involvement-in-primary-sjogrens-disease/