Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis-associated interstitial lung disease (RA-ILD) is heterogeneous with about half of patients having progressive disease. However, the rates of progression and the association of pulmonary function test (PFT) changes with subsequent lung transplant and ILD-related mortality are unclear. We determined the prevalence and outcomes for forced vital capacity percent predicted (FVCpp) decline among patients with RA-ILD.
Methods: We identified patients with RA-ILD in a large, multihospital healthcare system in the USA. All patients met 2010 ACR/EULAR classification criteria for RA and had clinically apparent RA-ILD. RA-ILD diagnosis was determined by review of high-resolution computed tomography (HRCT) imaging by up to 3 thoracic radiologists. We collected FVCpp measurements, covariates, and outcomes (lung transplant and ILD-related death) from the medical record. We used a relative FVCpp decline cutoff of >10% within 24 months. We also used a group-based trajectory model to obtain patterns of FVCpp change from RA-ILD diagnosis. The change from initial FVCpp was fitted and grouped using a maximum likelihood method. We then assessed for associations of each FVC decline definition with risk of subsequent lung transplant or ILD-related death using multivariable logistic regression, adjusted for age, sex, HRCT ILD pattern, and baseline FVCpp.
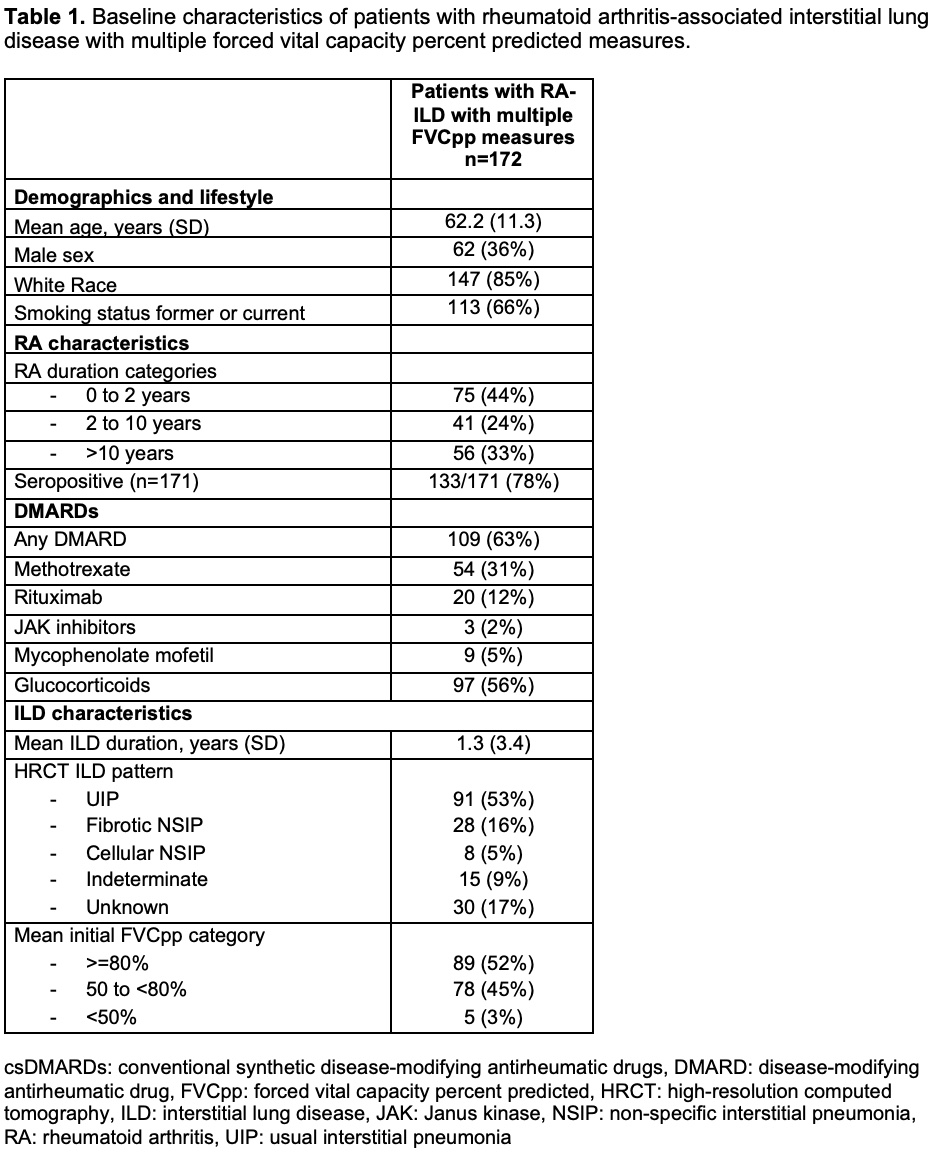
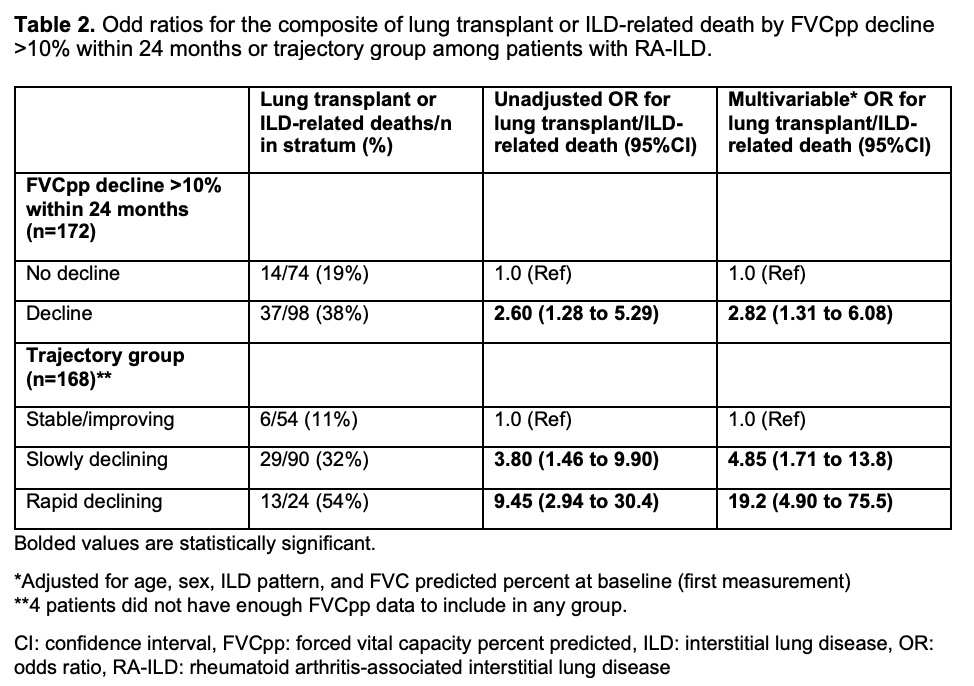
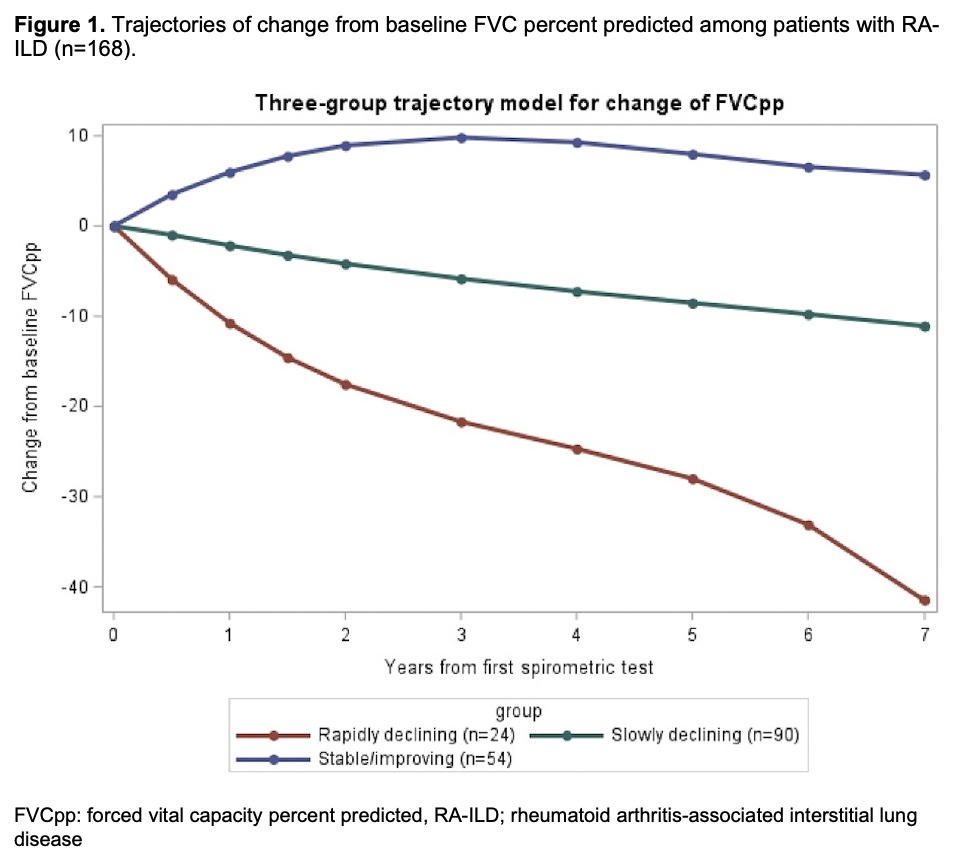
Results: We analyzed 172 patients with RA-ILD (mean age 62.2 years, 36% male) with a median of 6 FVCpp measurements per patient over 6.5 years of follow-up (Table 1). There were 7 (4%) lung transplants and 44 (26%) ILD-related deaths. 98 (57%) patients had relative decline of FVCpp by >10% over 24 months. These patients had an OR for lung transplant/ILD-related death of 2.82 (95%CI 1.31 to 6.08) compared to those that did not have >10% decline (Table 2). We identified 3 trajectory groups of FVCpp change: rapidly declining (n=24/168 [14%]), slowly declining (n=90/168 [54%]), and stable/improving (n=54/168 [32%]), Figure 1. Compared to the stable/improving group, the rapidly declining and slowly declining groups had ORs for lung transplant/ILD-related death of 19.2 (95%CI 4.9 to 75.5) and 4.85 (95%CI 1.71 to 13.8), respectively, Table 2.
Conclusion: Over half of RA-ILD patients had FVCpp decline defined by relative FVCpp decline >10% or the novel data-driven trajectory groups. The trajectory group approach identified three groups with different FVCpp trajectories, and the two declining groups had stronger associations with lung transplant or ILD-related death than the FVCpp >10% decline definition. The different trajectory groups demonstrate the heterogeneity within RA-ILD progression and the importance of PFT monitoring for identifying RA-ILD patients at the highest risk of poor outcomes.
To cite this abstract in AMA style:
Venkat R, Hayashi K, Juge P, McDermott G, Paudel M, Wang X, Vanni K, Kowalski E, Qian G, Bade K, Saavedra A, Mueller K, Chang S, Dellaripa P, Weinblatt M, Shadick N, J Doyle T, Dieudé P, Sparks J. Forced Vital Capacity Trajectories and Risk of Lung Transplant and ILD-Related Mortality Among Patients with Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/forced-vital-capacity-trajectories-and-risk-of-lung-transplant-and-ild-related-mortality-among-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/forced-vital-capacity-trajectories-and-risk-of-lung-transplant-and-ild-related-mortality-among-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease/