Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with rheumatoid arthritis (RA) have approximately a twofold increased risk of developing herpes zoster (HZ) compared to the general population. This elevated risk is attributed to the disease itself and related therapies used to manage RA, such as steroids, biologic modified anti-rheumatic drugs (bDMARDs), and targeted synthetic dmards (tsDMARD). In this health care cost study we aimed to measure health care utilization (HCU) and related costs of HZ infections among RA patients from the health care payer perspective.
Methods: Patients with RA were identified from the Ontario Rheumatoid Arthritis Database (ORAD), a population-based registry assembled using a validated algorithm, housed at ICES. Costs were measured from a single universal payer (Ontario Health Insurance Plan) at the patient level, with inpatient visits costed using capitation costing methodology. We included all adult (≥18 years) patients diagnosed with HZ between Jan 1, 2008, and March 31, 2020 (RA with HZ). A matched (control) cohort was identified and included all Ontario RA patients that were not diagnosed with HZ (RA without HZ) during the same period of time. The two cohorts were matched based on sex, date of birth (+/- 3 years) and index date (+/- 60 days of HZ infection). The primary outcome was total HCU cost (in Canadian Dollars) per year, up to 10 years of follow-up (adjusted for 2022 inflation). We also looked at the total number of clinical events (CEs) including the number of hospital admissions, emergency department visits, physician visits and other HCU. The two cohorts were compared using unadjusted gamma distribution models to assess HCU costs, and unadjusted generalized estimating equations (GEEs) with negative binomial distribution to assess total CEs.
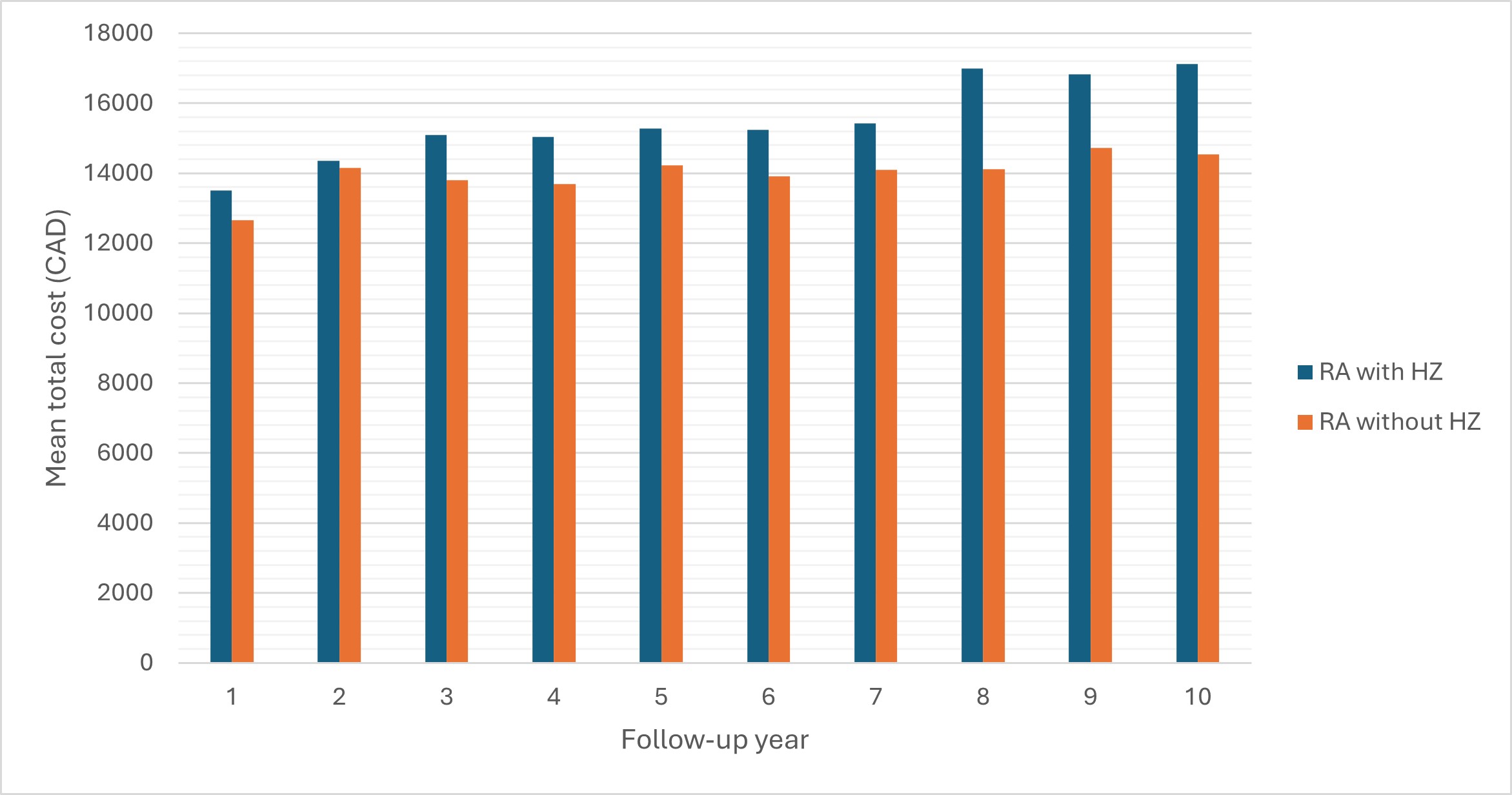
Results: We identified 15,573 RA patients diagnosed with HZ. The same number of RA patients without a HZ diagnosis were matched to this cohort. The RA with HZ cohort had significantly higher total HCU costs across all 10 years of follow-up (except year 2) compared to the RA without HZ cohort (Figure 1, p< 0.05). The mean total cost ranged from 13,507 CAD at year 1 to 17,120 CAD at year 10 for the RA with HZ cohort compared to 12,651 to 14,534 CAD in the RA without HZ cohort. Physician billing costs and inpatient hospital costs were the largest cost drivers for both cohorts.
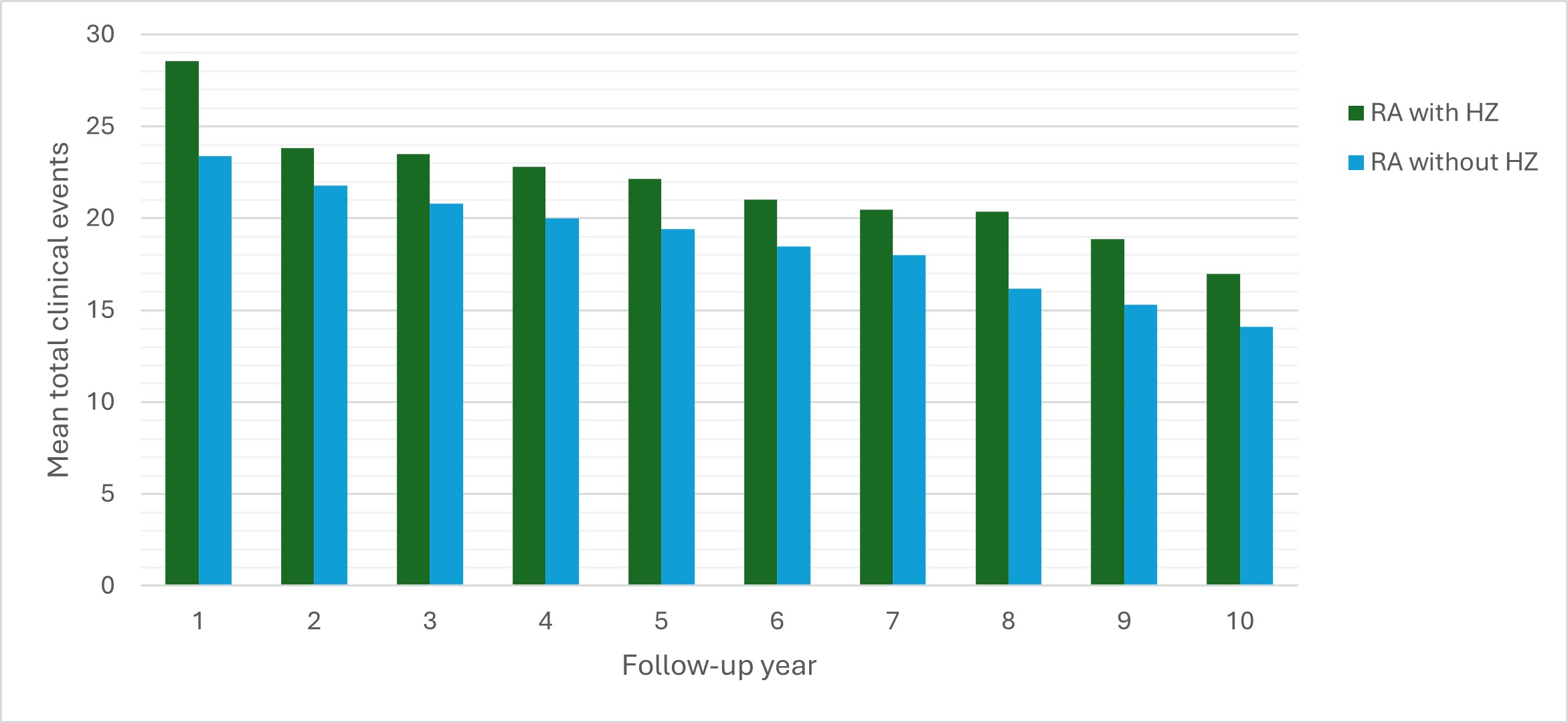
Compared to RA patients with HZ, matched RA patients without HZ experienced a significantly lower mean number of total CEs (Figure 2, p< 0.05). The difference in total CEs between cohorts, was the highest one year following a HZ infection. The mean total number of CEs was 28.56 for the RA with HZ cohort compared to 23.4 in the RA without HZ cohort. Physician visits were the main driver for clinical events over the 10 years of follow-up.
Conclusion: In this study we found that HCU costs and total CEs were higher in RA patients with HZ compared to RA patients without HZ. Thus, rheumatologists should consider treatment strategies that minimize the risk of HZ and ensure patients’ vaccinations are up to date.
To cite this abstract in AMA style:
Movahedi M, Cesta A, Li X, Tatangelo M, Bombardier C. Health Care Utilization and Cost of Herpes Zoster Infection in Patients with Rheumatoid Arthritis, a Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/health-care-utilization-and-cost-of-herpes-zoster-infection-in-patients-with-rheumatoid-arthritis-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/health-care-utilization-and-cost-of-herpes-zoster-infection-in-patients-with-rheumatoid-arthritis-a-retrospective-cohort-study/