Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: In recent years, connective tissue diseases (CTDs) have been increasingly recognized as a significant underlying pathology of interstitial lung diseases (ILDs). Amongst CTDs, idiopathic inflammatory myopathies (IIMs) are characterized by a high prevalence of pulmonary insult, which may also be the first clinical manifestation, preceding musculoskeletal complaints. The detection of myositis-specific and associated autoantibodies (MSAs/MAAs) has aided in IIM diagnosis and categorization of myositis patients with distinct clinical features. In this study, we aimed to determine the prevalence of MSAs/MAAs in consecutive ILD patients of unknown etiology, as well as identify potential clinical associations
Methods: 83 consecutive ILD patients followed in Sotiria, Naval Hospital, Laiko and Attiko General Hospitals, in Athens, Greece, were referred for MSA/MAA autoantibody testing by immunoblot assay in Molecular Physiology and Clinical Applications Unit, Department of Physiology, National and Kapodistrian University of Athens, after infection was excluded. Complete rheumatologic evaluation was also performed. Mann-Whitney and chi-squared tests were used to draw two-group comparisons for continuous and categorical data respectively. Bulk RNA-sequencing was performed in 10 RNA samples (3 MDA5+, 4 anti-synthetase + and 3 Pm/Slc+), on an Illumina NextSeq550 platform and appropriate bioinformatics analysis was performed.
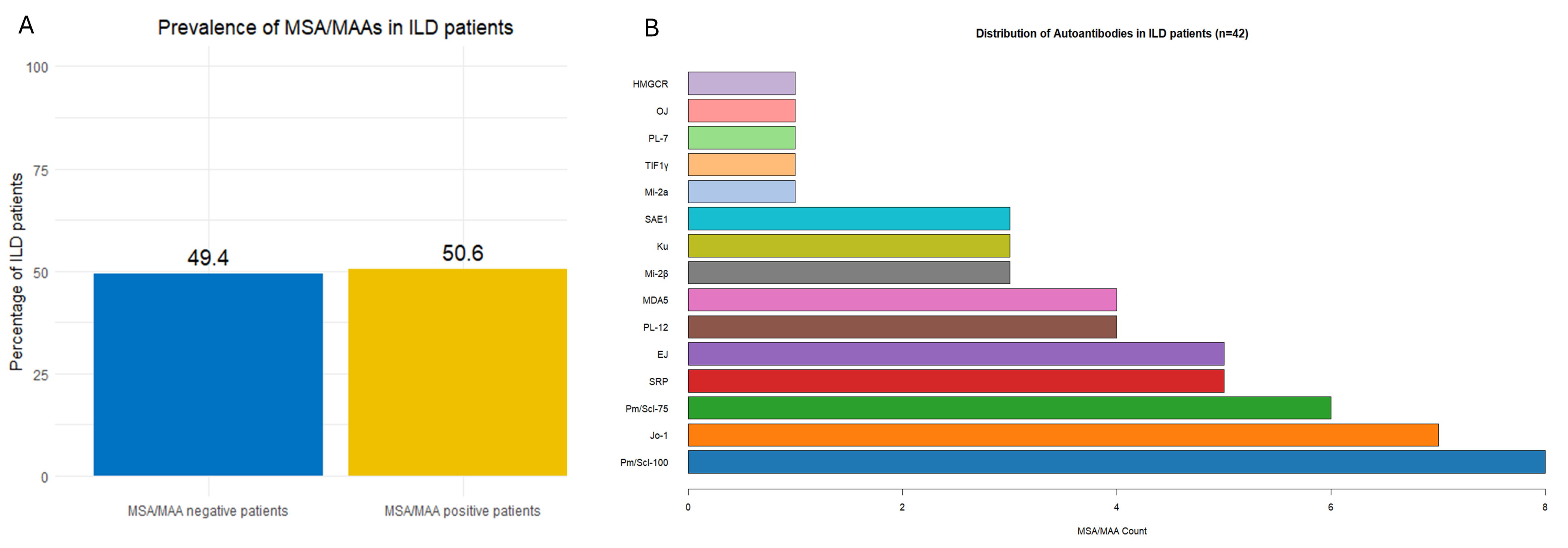
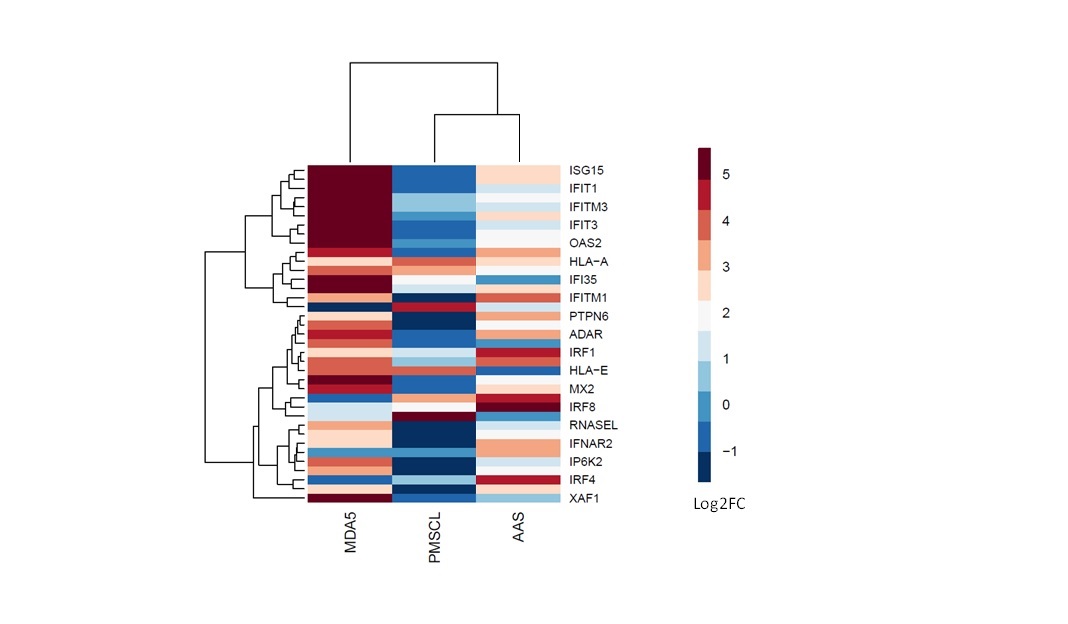
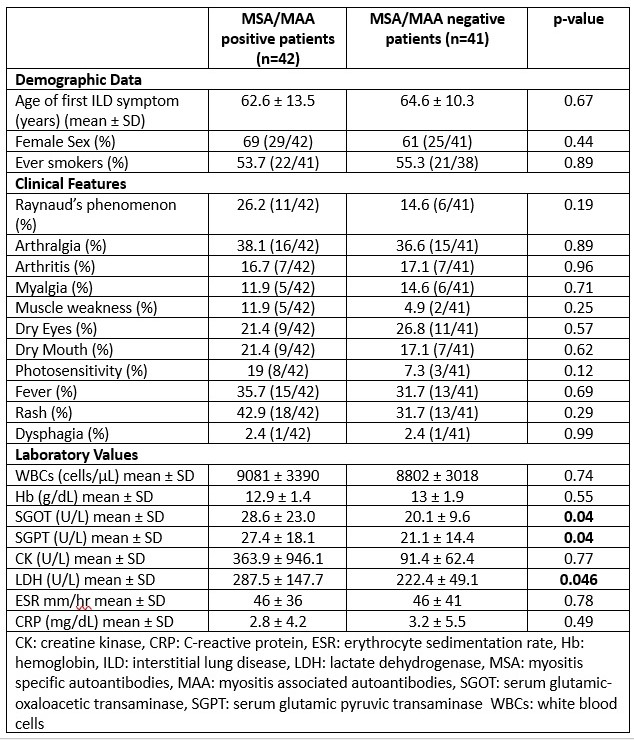
Results: In this ILD patient cohort, the prevalence of MSAs/MAAs was 50.6% (Figure 1A). Eleven patients were positive for more than one autoantibody. The distribution of the autoantibodies detected was as follows: Pm/Scl-100 (n=8), Jo-1 (n=7), Pm/Scl-75 (n=6), SRP and EJ (n=5), PL-12 and MDA-5 (n=4), Mi-2β, Ku and SAE-1 (n=3), Mi-2α, TIF-1γ, PL-7, OJ and HMGCR (n=1) (Figure 1B). There were no significant differences in clinical features between antibody positive and antibody negative patients, though seropositive patients displayed higher levels of liver enzymes and lactate dehydrogenase (Table 1). Based on radiological findings, the ILD patterns of this cohort consisted of 25 patients with usual interstitial pneumonia (UIP), 16 with non-specific interstitial pneumonia (NSIP), 23 with organizing pneumonia (OP), 4 with NSIP/OP, and 15 with interstitial lung abnormalities. Interestingly, patients with ILD and MDA5+ autoantibodies exhibited the greatest overexpression of type I IFN inducible genes compared to the other groups as seen in the heatmap (Figure 2)
Conclusion: MSAs/MAAs are frequently detected in patients with ill-defined ILD. Early detection of autoimmunity through MSA/MAA testing may allow for improved management strategies in ILD, potentially leading to better clinical outcomes. Additionally, distinct autoantibody groups exhibit variable type I IFN inducible gene expression profiles. Further investigations with larger patient cohorts are warranted
To cite this abstract in AMA style:
Koulouri V, Voulgareli I, Flouda S, Galanopoulou N, Marketos N, Skarlis C, Raftopoulou S, Tavernaraki K, Chronaiou A, Tsoukalas G, Zias N, Boumpas D, Mavragani C. Increased Prevalence of Myositis Specific and Associated Autoantibodies in Patients with Interstitial Lung Disease of Unknown Etiology [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-prevalence-of-myositis-specific-and-associated-autoantibodies-in-patients-with-interstitial-lung-disease-of-unknown-etiology/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-prevalence-of-myositis-specific-and-associated-autoantibodies-in-patients-with-interstitial-lung-disease-of-unknown-etiology/