Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
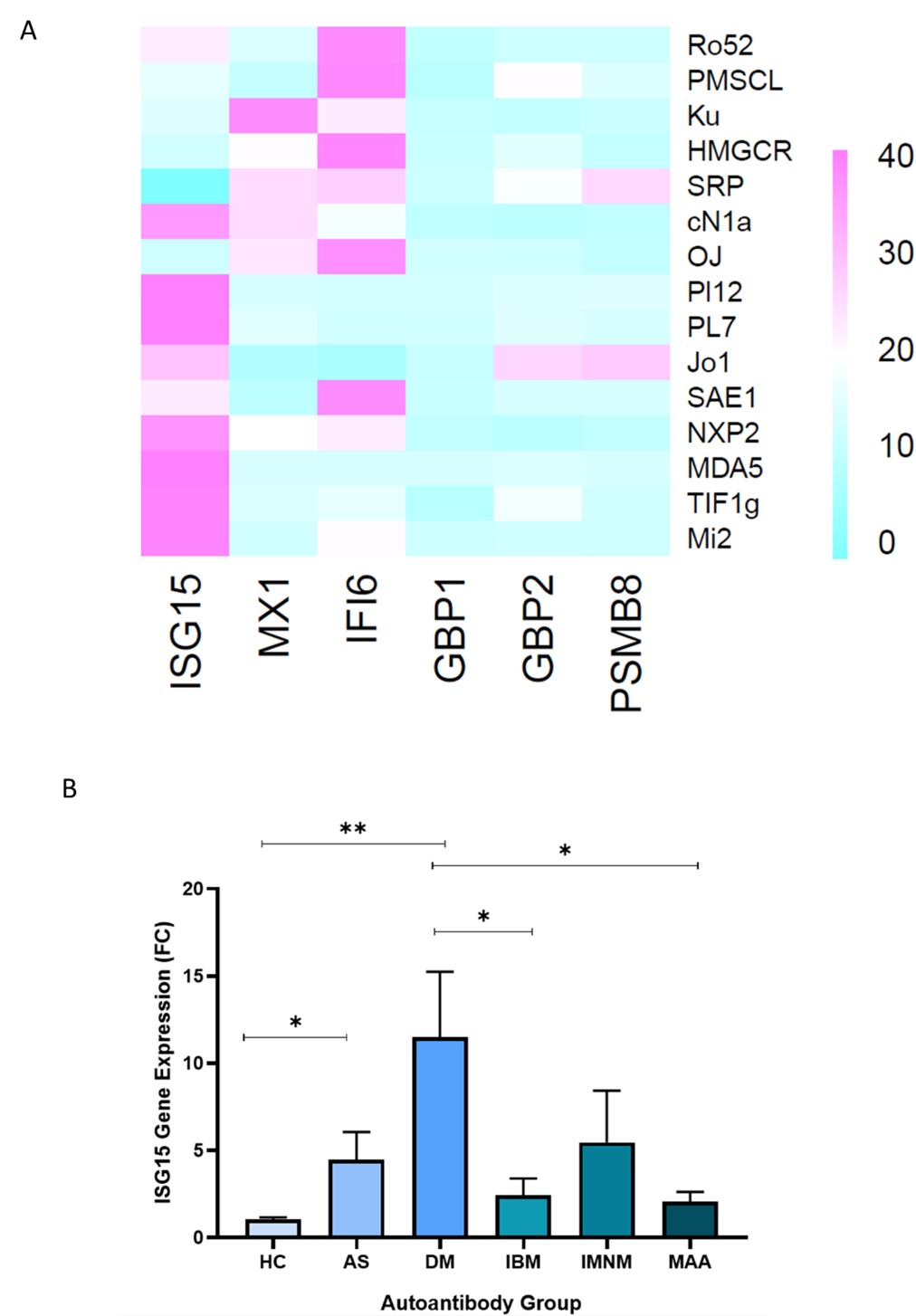
Background/Purpose: Idiopathic inflammatory myopathies (IIM) are characterised by muscle inflammation (myositis) and weakness, impacting various organ systems. Clinical subtypes include dermatomyositis (DM), antisynthetase syndrome (ASyS), immune-mediated necrotising myopathy (IMNM) and inclusion body myositis (IBM). Myositis-specific and -associated autoantibodies (MSAs/MAAs) have been used in clinical practice as they are closely associated with distinct clinical phenotypes of IIM and can be used as confirmatory diagnostic tools. Interferons (IFNs) have been shown to play a central role in IIMs and particularly in the inflammatory process which characterises IIMs. IFN stimulated genes (ISGs) induced by type I IFN have an established role in DM and are significantly involved in patients with DM, positive for anti-melanoma differentiation-associated gene 5 (MDA5) autoantibodies. ISGs induced by type II IFN have been shown to be upregulated in IBM and ASyS while it is yet unclear whether IFNs play a substantial role in IMNM. In muscle biopsies, ISG15, IFI6, and MX1 were the most upregulated ISGs in DM and PSMB8, GBP1 and GBP2 were the most upregulated ISGs in ASyS and IBM, highlighting the predominant involvement of both type I and II ISGs in different IIM clinical subtypes. However, muscle biopsies are estimated to have a false negative rate of 23%, while they also constitute an invasive procedure which is difficult to be repeated longitudinally in the context of a follow-up. A thorough clinical examination, coupled with the presence of MSAs or MAAs and the occasional verification via magnetic-resonance imaging can suffice to reach a diagnosis, digressing from the need to perform muscle biopsies. We aimed to investigate the type I and II IFN profiles in the peripheral blood of patients with IIM features who were seropositive for MSAs or MAAs.
Methods: 124 peripheral blood samples, stored in the Biobank of Molecular Physiology and Clinical Applications Unit, Department of Physiology from seropositive patients for MSA or MAA autoantibodies detected by a commercial immunoblot kit (EUROIMMUN) were subjected to RNA extraction, cDNA synthesis and qPCR for the quantitation of the following genes: ISG15, IFI6, MX1, PSMB8, GBP1 and GBP2. Patients provided their written informed consent while samples were collected at baseline and are treatment-naïve.
Results: We showed that the expression of ISG15, MX1 and IFI6 is more prevalent than that of GBP1, GBP2 and PSMB8 in patients positive for MSAs or MAAs. Specifically, ISG15 expression was highest in patients with DM related autoantibodies (Mi2, NXP2, TIF1g, MDA5) and to a lesser extent in patients with ASyS (particularly PL7, PL12) (Figs 1A&B). The expression of ISG15 was 3.5 times greater (p=0.001) in patients who presented with muscle weakness than those who did not. Patients who presented with dysphagia had 3.8 times greater ISG15 expression (p=0.001) than those who had no such symptom.
Conclusion: In conclusion, ISG15 peripheral blood expression was found to be predominantly upregulated in seropositive patients characterized by the presence of DM related autoantibodies and therefore could serve as a noninvasive biomarker potentially guiding a tailored therapeutic approach.
To cite this abstract in AMA style:
Raftopoulou S, Michalakeas N, Gerochristou M, Marketos N, Skarlis C, Mavragani C. Increased ISG15 Expression in Peripheral Blood from Patients with Positive Dermatomyositis Related Specific Autoantibodies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-isg15-expression-in-peripheral-blood-from-patients-with-positive-dermatomyositis-related-specific-autoantibodies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-isg15-expression-in-peripheral-blood-from-patients-with-positive-dermatomyositis-related-specific-autoantibodies/