Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with early inflammatory arthritis (EIA) need to be seen urgently to initiate treatment. Our community rheumatology clinic in Ontario, Canada was concerned that EIA cases may be delayed unnecessarily if referrals lacked sufficient detail to triage accurately. In a prior quality improvement project, we redesigned our triage process to include a patient survey (the “EIA Tool”), which was validated to identify referrals with EIA. In this study, we aimed to evaluate the sensitivity and specificity of the new triage process for referrals with unclear urgency after 12 months of use.
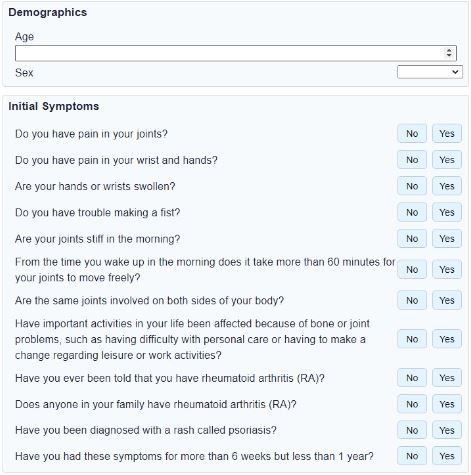
Methods: All referrals accepted by one rheumatologist were included from April 2020-July 2022. During the intervention period, we implemented the new triage process. The rheumatologist triaged all referrals as urgent, non-urgent, or unclear. Patients with unclear urgency were asked to complete the online EIA Tool (Figure 1) prior to scheduling. Their survey result determined a triage score of urgent or non-urgent, and consultations were scheduled accordingly. Post-consultation, the rheumatologist determined the ‘true’ urgency score, while blinded to the pre-consultation score. Data were collected prospectively on all incoming referrals. We analyzed the data using descriptive statistics and calculated the sensitivity and specificity of the baseline and new triage processes.
Results: The 16-month baseline period (April 2020 to July 2021) included 1296 referrals; 647 (50%) were triaged as urgent. The 12-month intervention period (August 2021-July 2022), included 888 referrals; 508 (57%) were triaged as urgent, and 97 (11%) were triaged as unclear. The EIA tool was completed in all unclear cases; 93 patients submitted the survey online, and 4 patients without email completed the survey by phone. Most patients (86%) completed the survey within 1 day of receiving it. Unclear cases had a cycle time from referral to scheduling of 5 days, compared to 3 days for those who were not sent the EIA tool. The sensitivity to identify urgent cases was 97% during the intervention versus 85% at baseline. The specificity during the intervention was 59% versus 70% at baseline.
Conclusion: The EIA Tool helped us detect 97% of truly urgent cases, thereby reducing the risk of delayed treatment caused by triage error. We have since spread this process to four rheumatologists in our clinic. Our next step is to analyze urgent referral volume using statistical process control charts, in order to modify our scheduling algorithm.
To cite this abstract in AMA style:
Gottheil S, Gottheil C, Carson J. Improving Triage Accuracy of Unclear Rheumatology Referrals: A Quality Improvement Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/improving-triage-accuracy-of-unclear-rheumatology-referrals-a-quality-improvement-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-triage-accuracy-of-unclear-rheumatology-referrals-a-quality-improvement-study/