Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Although urinary symptoms are often reported by people with SLE and may substantially affect quality of life, little is known about the burden of urinary incontinence (UI) in people with SLE. Our primary objective was to estimate its burden among a predominantly Black, population-based U.S. cohort of adults with SLE. Secondarily, we sought to understand the association of SLE activity and related organ damage with UI in this population.
Methods: Participants were recruited for a one-time visit (10/2019-5/2022) from an ongoing population-based cohort of adults meeting validated criteria for SLE in metropolitan Atlanta [Georgians Organized Against Lupus (GOAL)]. Participants self-reported presence, type, severity, and frequency of UI over the last 12 months, as well as amount of bother from UI and its effect on activities of daily living (ADLs), via an adapted National Health and Nutrition Examination Survey instrument. SLE activity was measured via the Systemic Lupus Activity Questionnaire (SLAQ; higher scores = higher disease activity). Cumulative SLE-associated overall organ, neuropsychiatric, and musculoskeletal damage were determined via the Brief Index of Lupus Damage (BILD; higher scores = greater degree of SLE-mediated organ damage). We evaluated the associations of SLAQ and BILD scores, as well as musculoskeletal and neuropsychiatric damage, with UI (defined as any leakage at least a few times a month over the last 12 months) using multivariable logistic regression adjusting for demographic (age, sex, race, education) and clinical (disease duration, body mass index) characteristics and reported adjusted odds ratios [aOR] and 95% CIs.
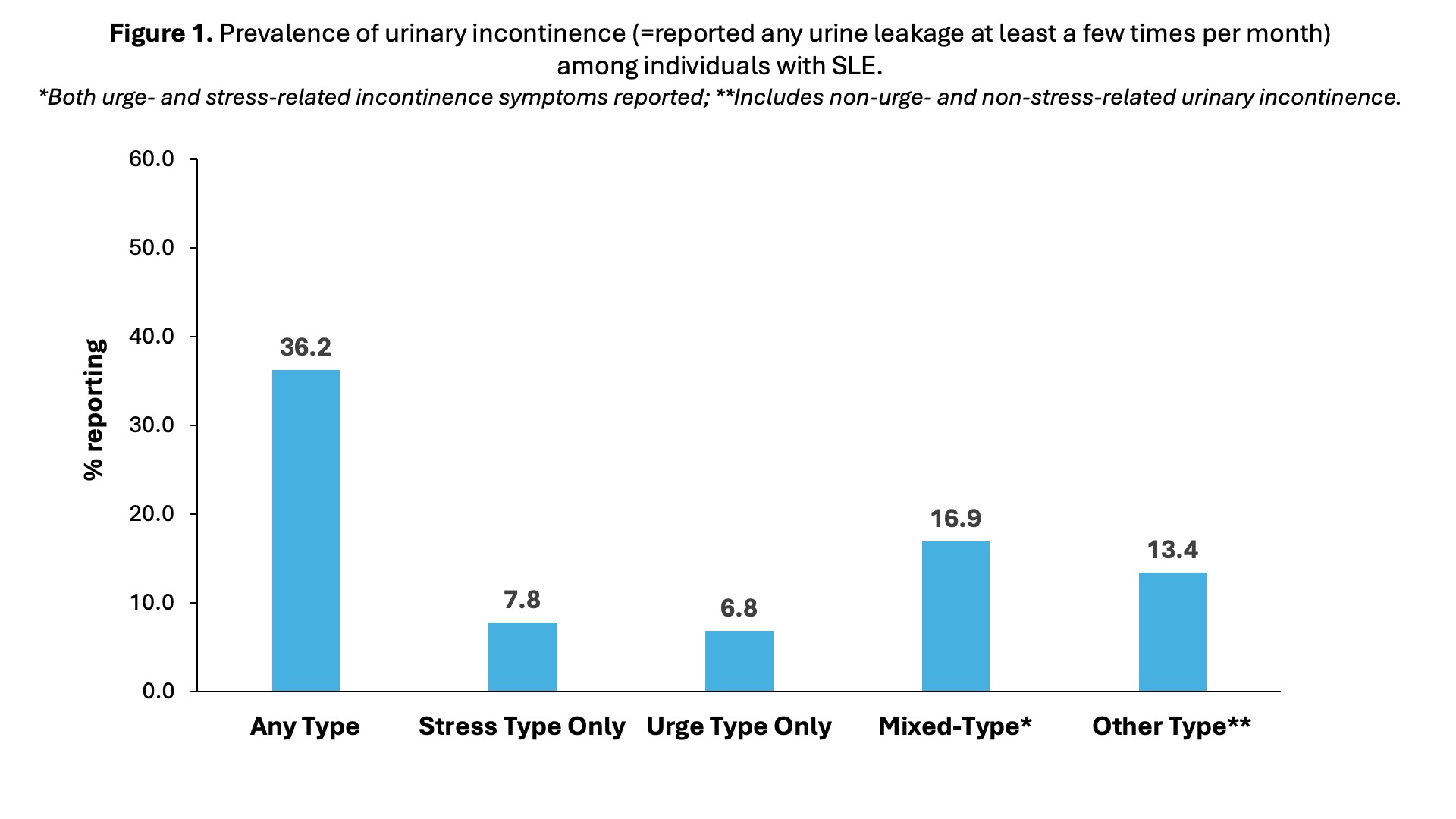
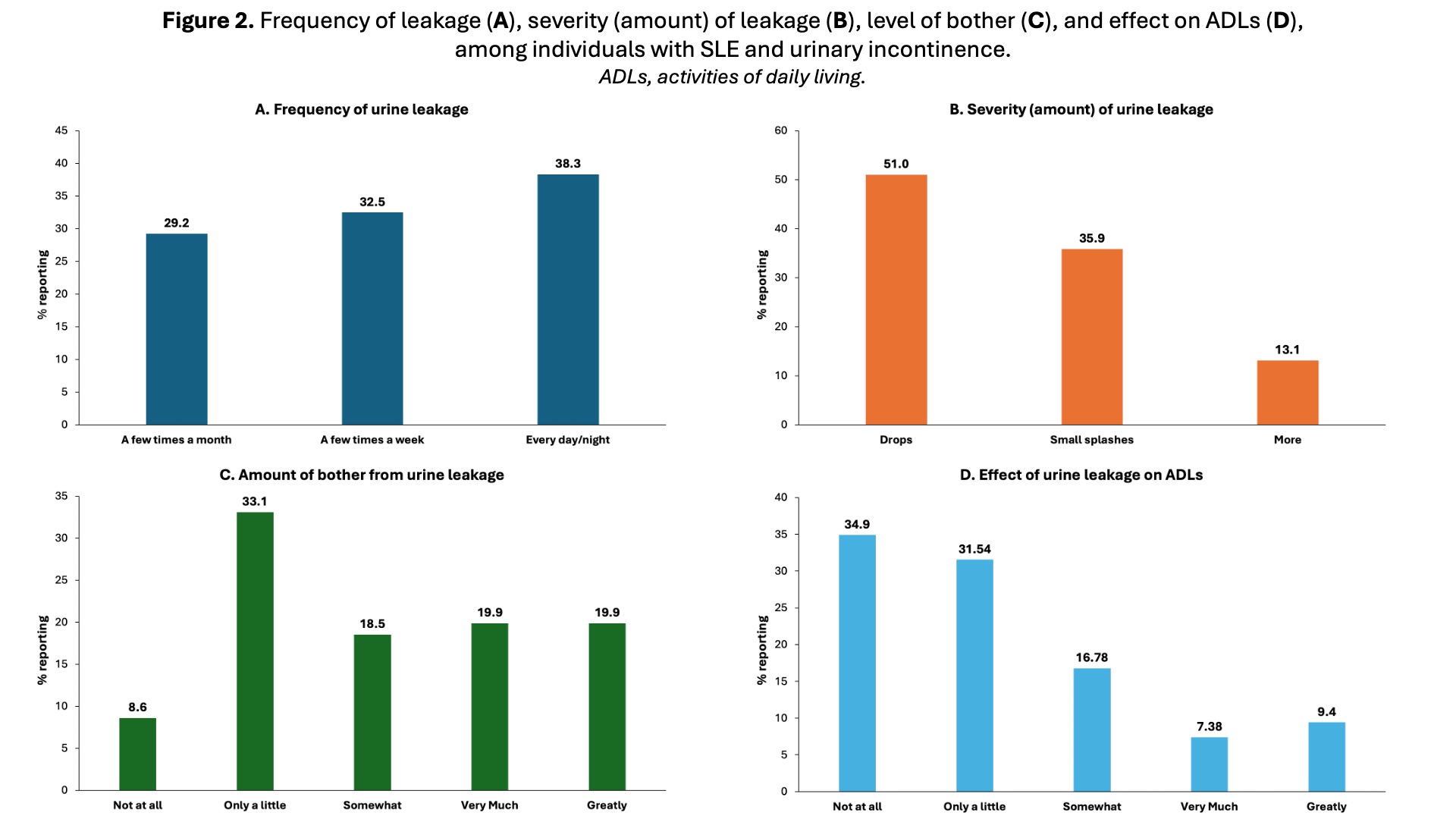
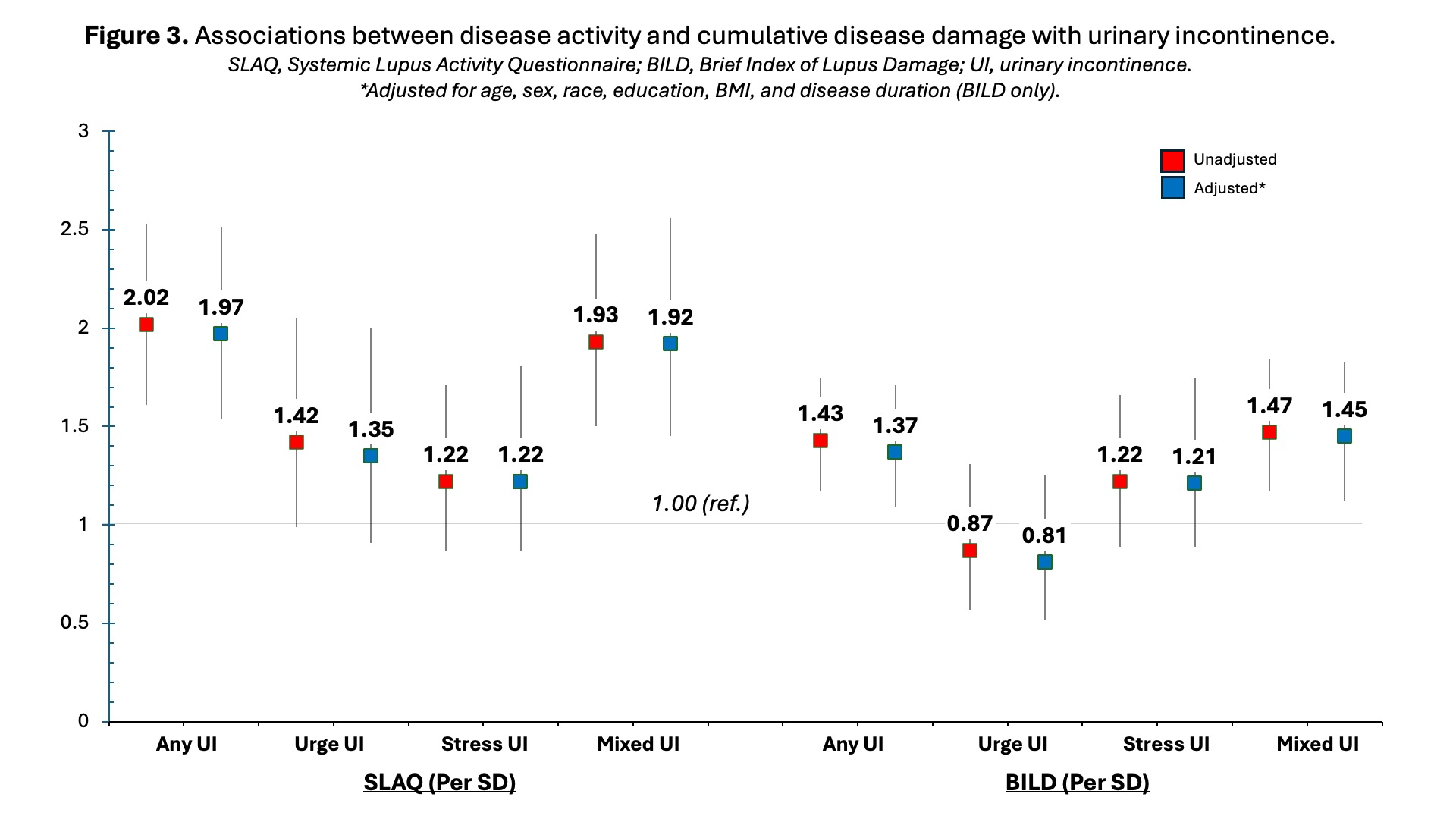
Results: Among N=425 participants who completed the questionnaire (mean age, 46.2; 91.7% female; 81.9% Black; median participant SLAQ and BILD scores, 11 and 2), more than one-third (36.1%) reported UI, with mixed-type UI being most common (Figure 1). Most (60.8%) participants with UI experienced leakage at least a few times a week (Figure 2A), with nearly half (49.0%) noting more than small drops with urine leakage (Figure 2B). Participants with UI commonly reported that it bothered them (39.7%) (Figure 2C) and affected their ADLs (18.8%) (Figure 2D) very much or greatly. After full adjustment, higher disease activity was associated with 2.0- and 1.9-fold higher odds of any and mixed UI, respectively; while SLE-associated organ damage was associated with 37% and 45% higher odds of any and mixed UI (Figure 3). Neuropsychiatric (but not musculoskeletal) damage was statistically significantly associated with increased odds of any (aOR 2.20, 95% CI 1.22-3.94) and mixed (aOR 3.21, 95% CI 1.62-6.35) types of UI.
Conclusion: Prevalence of UI among those with SLE may be high relative to the general U.S. adult population (~33%). The burden of UI, in terms of severity, frequency, and effect on individuals, was substantial in this study. Clinicians should consider screening for UI among SLE patients, particularly those with greater disease activity or neuropsychiatric damage. Further research is necessary to identify at-risk individuals and effective strategies for managing UI and its associated burden for individuals with SLE.
To cite this abstract in AMA style:
Salazar G, Yazdany J, Hoge C, Lim S, Bauer S, Plantinga L. Urinary Incontinence Among Individuals with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/urinary-incontinence-among-individuals-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/urinary-incontinence-among-individuals-with-systemic-lupus-erythematosus/