Session Information
Date: Saturday, November 16, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Giant Cell Arteritis (GCA) poses diagnostic challenges, especially in rural areas, where limited access to healthcare can delay diagnosis and worsen outcomes, a concern not yet explored in GCA. This knowledge gap underscores the need for research on the impact of rurality on GCA diagnosis, which is crucial for improving patient prognosis and addressing the potential $76 billion cost associated with GCA-related visual loss in the aging US population. We compared characteristics of non-rural and rural GCA patients, and determined factors associated with time to GCA diagnosis in a large single-center cohort.
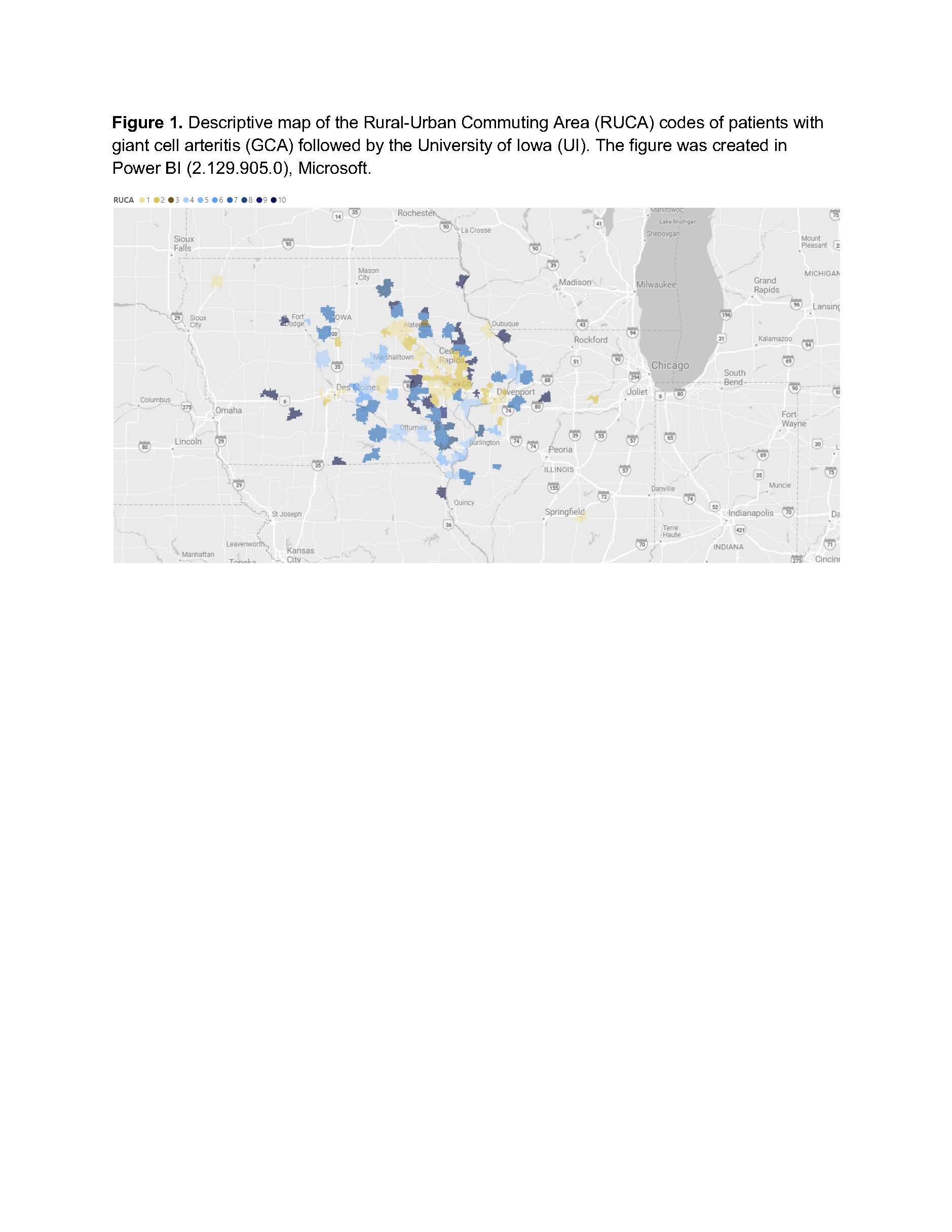
Methods: Adults with GCA meeting the 2022 EULAR/ACR GCA classification criteria and followed in the University of Iowa (UI) rheumatology clinics from 2/1/2000 to 2/7/2024 were included in this cross-sectional analysis. Data was abstracted from UI’s electronic medical record for demographics, disease features, and diagnostic studies. Geographic categories were defined by the Rural-Urban Commuting Area (RUCA) codes 2010, categorizing home addresses from metropolitan to rural areas (ranges from 1-10).
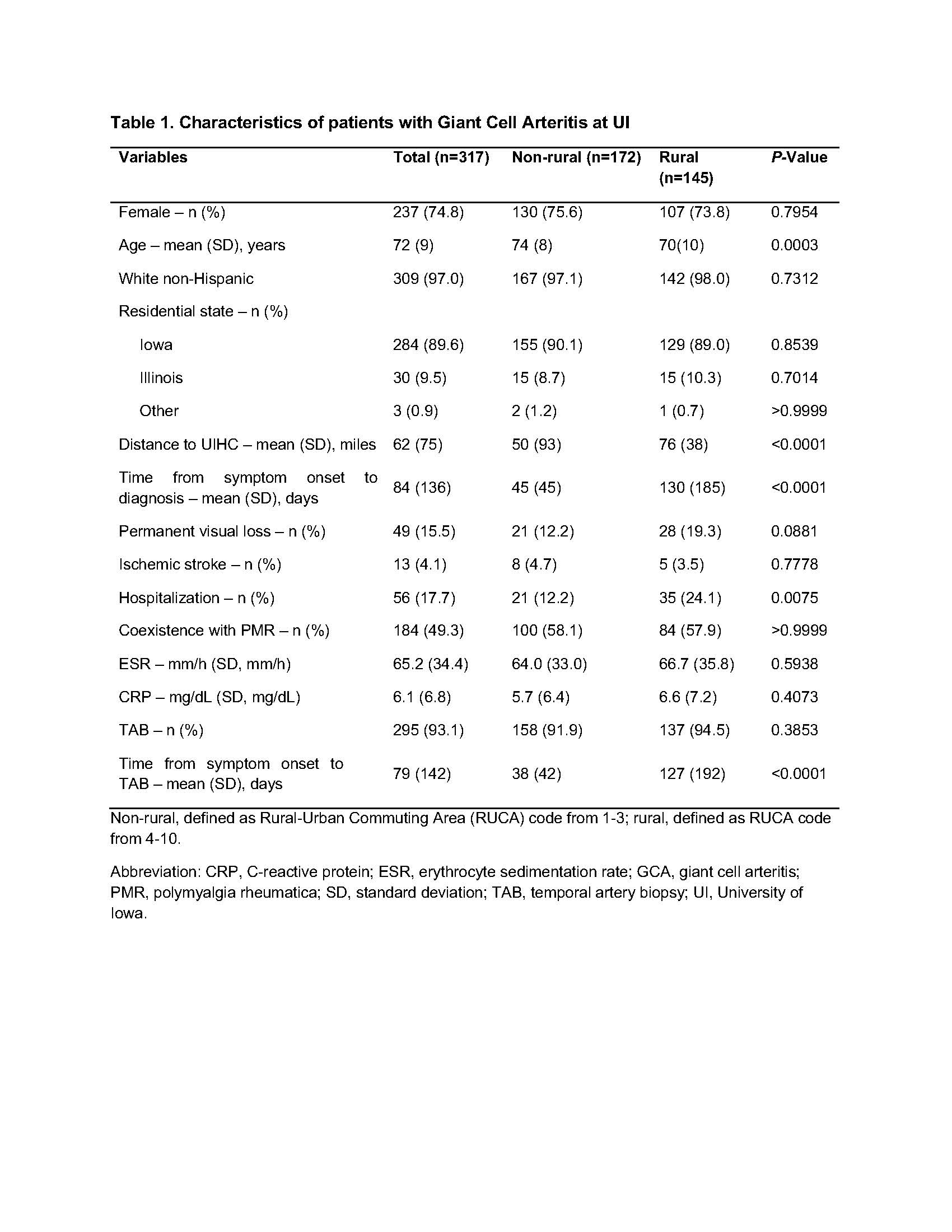
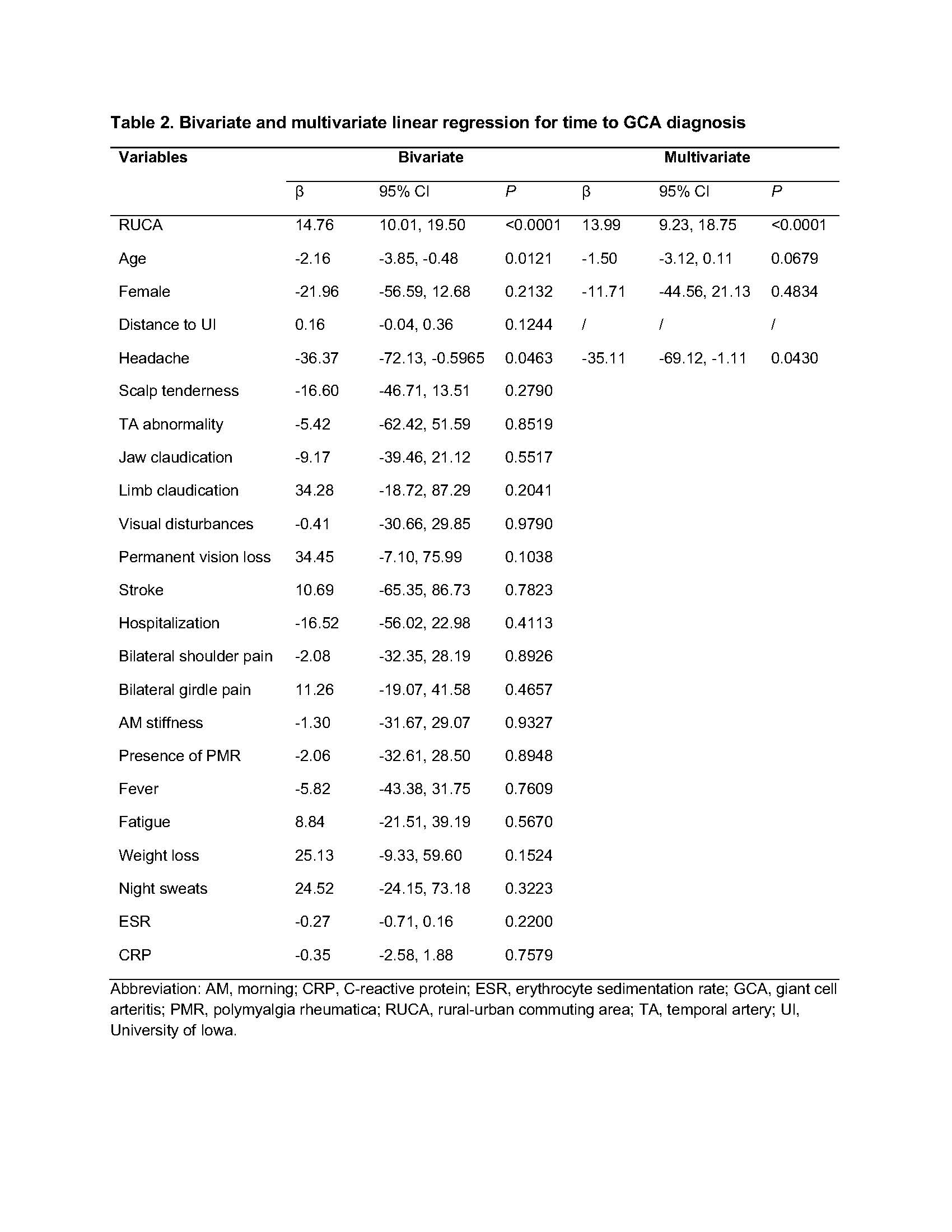
Patient characteristics were expressed as means or proportions. First, we compared characteristics of non-rural (RUCA 1-3) and rural (RUCA 4-10) GCA patient groups. Differences between groups were evaluated with the t-test or Mann-Whitney U test for continuous variables, and the Chi-square or Fisher’s exact test for categorical variables. Second, for our primary outcome of interest (time to GCA diagnosis), we performed bivariable analyses between each predictor and time to GCA diagnosis with simple linear regression. Next, multivariable linear regression (MLR) models were fitted to identify the best predictors of time to GCA diagnosis.
Results: Baseline characteristics of 317 patients included in this study are shown in Table 1. In this predominantly female non-Hispanic white GCA cohort with a mean age of 72 (9) years, 54.3% resided in non-rural areas, while 45.7% resided in rural areas (Figure 1).
The mean time to GCA diagnosis was significantly increased in rural compared to non-rural GCA subjects (130±185 days vs 45±45 days, p< 0.0001) (Table 1). A higher rate of hospitalizations was observed among rural subjects (24.1% vs 12.2%, p=0.0075), and the mean time from symptom onset to temporal artery biopsy (TAB) was significantly increased in rural subjects (127±192 vs 38±42 days, p< 0.0001).
Bivariable analyses identified four variables (RUCA code, age, headache, distance to UI) associated with time to GCA diagnosis (p< 0.20). In MLR analyses, with biological sex forced into the model, three variables provided the best fit (adjusted-R2 0.1182, p< 0.001). With increasing RUCA code, the mean time to GCA diagnosis was increased. In contrast, the presence of headache decreased the mean time to GCA diagnosis.
Conclusion: Rurality was identified as the strongest predictor of delayed diagnosis in GCA. Additionally, rural patients experienced an increased time to temporal artery biopsy and higher proportion of hospitalizations. Future prospective studies are needed to assess the impact of rurality on clinical outcomes in GCA.
To cite this abstract in AMA style:
Ni R, Kumar B, Lenert A. Rurality and Delayed Diagnosis of Giant Cell Arteritis – a Single Center Experience [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/rurality-and-delayed-diagnosis-of-giant-cell-arteritis-a-single-center-experience/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rurality-and-delayed-diagnosis-of-giant-cell-arteritis-a-single-center-experience/