Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a heterogeneous group of rare diseases characterized by necrotizing inflammation predominantly of small vessels, with the presence of these circulating antibodies. AAV includes three major diseases: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). However, overlapping clinical phenotypes of AAV subgroups continually provoke controversies over the diagnostic and classification criteria. The objective of our work is to describe the phenotypic characteristics of ANCA-positive patients in a retrospective cohort and their clinical implications.
Methods: We conducted a retrospective observational study at a single center including patients over 18 years old with positive immunoassays for MPO-ANCA and/or PR3-ANCA over a seven-year period (January 2015 to December 2022). Patients were classified as having AAV according to the 2022 ACR/EULAR criteria. We analyzed demographic characteristics, ANCA titers at diagnosis, and primarily affected domains in cases of AAV. Statistical analysis was performed using R software.
Results: A total of 119 ANCA-positive patients were included. The average age of the sample was 63 ± 18 years, consisting of 59 women (49.6%) and 60 men (50.4%), 113 (94.95%) were Caucasian, and 6 were of Latin American origin (5.06%). We found that there were 47 cases (39.5%) of anti-PR3 type ANCA and 74 (62.2%) of anti-MPO type.
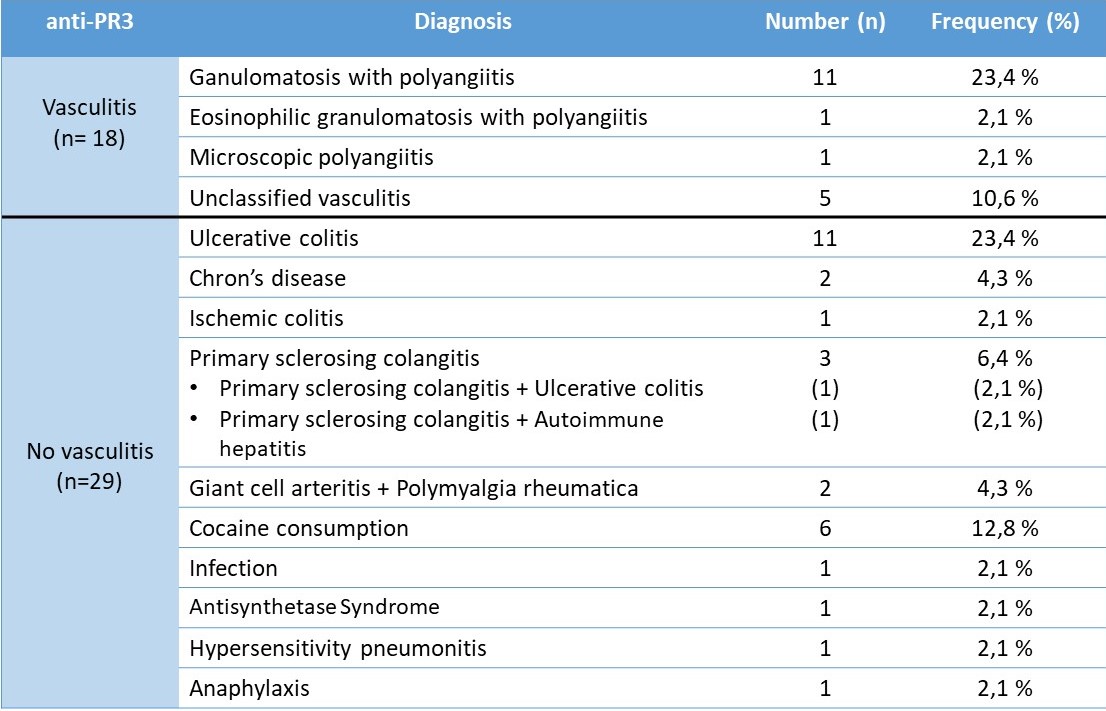
Within the anti-PR3 group, we differentiated the diagnoses listed in Table 1.
Regarding the primarily affected domains among patients with a confirmed diagnosis of vasculitis, pulmonary involvement was the most frequent (66.7%), followed by renal and otolaryngological (44.4%). Next were joint manifestations, present in 33.3%, and finally cutaneous (22.2%) and neurological (11.1%) manifestations.
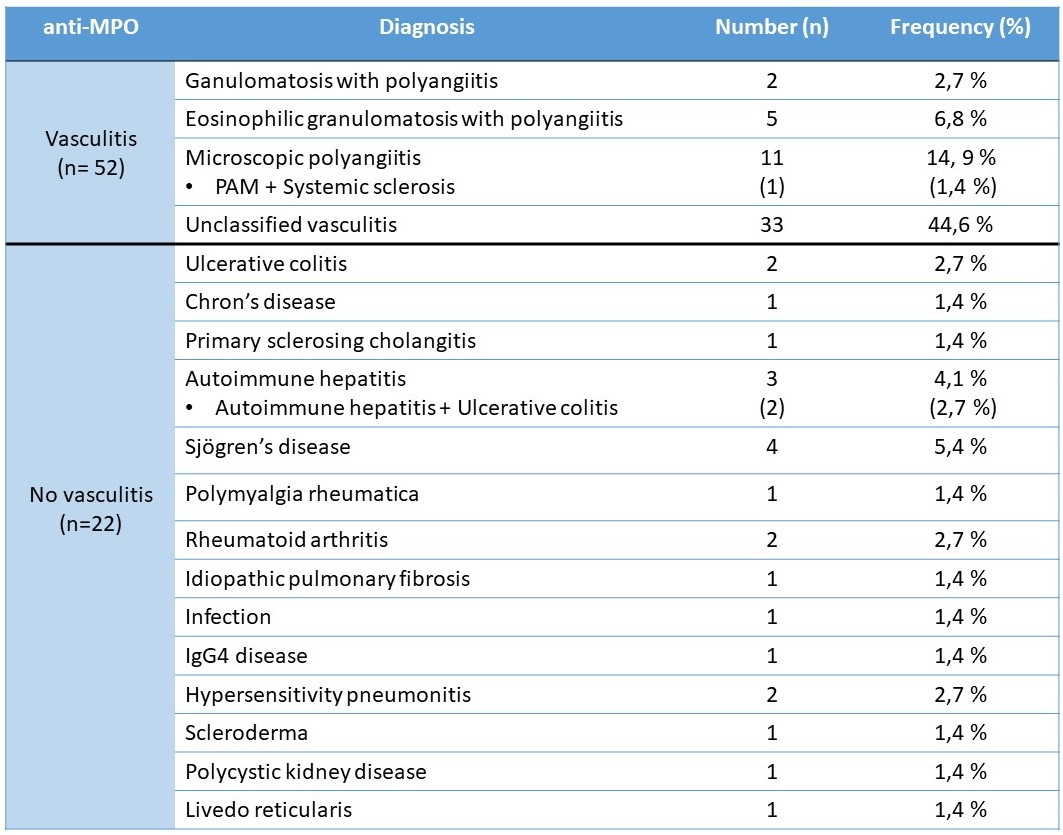
In the anti-MPO group, we found the diagnoses listed in Table 2.
In this group, the most prevalent domains affected were renal involvement in 73.1% of the patients, followed by pulmonary (57.7%), neurological (19.2%), and joint (17.3%). There was also involvement of the cutaneous (15.4%), hematological (7.7%), and otolaryngological (3.8%) domain.
In our sample, as in previous studies, at diagnosis, patients with higher ANCA titers were more likely to have AAV. PR3-ANCA showed greater sensitivity than MPO-ANCA for GPA (23.4% vs 2.7%, p = 0.9) and MPO-ANCA had greater sensitivity in MPA (14.9% vs 2.1%, p= 0.16), although it did not show statistical significance possibly due to the sample size.
Conclusion: In light of the results obtained, the presence of ANCA+ is not exclusive to systemic vasculitis, and other diagnostic possibilities must be considered, such as other autoimmune diseases, infections, and toxic exposures. However, high titers of ANCA (MPO or PR3) should suggest the presence of AAV. Patients positive for MPO-ANCA showed significantly more frequent renal involvement, followed by pulmonary and peripheral nervous system involvement. Meanwhile, patients positive for PR3-ANCA had a significantly higher prevalence of pulmonary involvement, followed by renal and otolaryngological involvement.
To cite this abstract in AMA style:
Sanmartín Martínez M, González Mazario R, Martínez Calabuig P, Salvador Maicas L, Lorente Betanzos I, Fragío Gil J, Molina Almela C, Rueda A, Lerma Garrido j, Sierra Rivera A, Campos Fernández C. Antineutrophil Cytoplasmic Antibodies and Associated Vasculitis According to Clinical Phenotypes: A Single-Center Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/antineutrophil-cytoplasmic-antibodies-and-associated-vasculitis-according-to-clinical-phenotypes-a-single-center-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antineutrophil-cytoplasmic-antibodies-and-associated-vasculitis-according-to-clinical-phenotypes-a-single-center-retrospective-cohort-study/