Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Glial fibrillary acidic protein (GFAP), an intermediate filament protein produced by astrocytes in the CNS, has been identified as a biomarker for disease activity in various CNS diseases. Given its potential production in other major organs and differential regulation in inflammatory conditions, it is hypothesized that serum GFAP could estimate vasculitis activity in antineutrophil cytoplasmic antibody-associated vasculitis (AAV). This study aims to explore whether serum GFAP can serve as a biomarker for estimating cross-sectional vasculitis activity in AAV patients.
Methods: Eighty AAV patients were selected from the SHAVE (Severance Hospital ANCA-associated VasculitidEs) cohort at Severance Hospital, meeting criteria including initial AAV diagnosis, adherence to the international classification criteria, including the 2022 ACR/EULAR classification criteria, and comprehensive medical records. The exclusion criteria included serious mimicking conditions and unavailable serum samples. Seventy-four patients were ultimately included.
Clinical data collected included demographic details, AAV subtype, ANCA type and positivity, BVAS, five-factor score (FFS), short form survey (SF-36) scores, vasculitis damage index (VDI), and comorbidities such as diabetes, hypertension, and dyslipidemia. Follow-up data included all-cause mortality and progression to end-stage kidney disease (ESKD) and immunosuppressive drug usage frequency. Serum GFAP levels were measured using an ELISA kit.
Statistical analyses were performed by SPSS, using median values for continuous variables and percentages for categorical variables. Pearson correlation, ROC curve analysis, chi-square tests, and Kaplan-Meier survival analysis were employed, with p< 0.05 considered statistically significant.
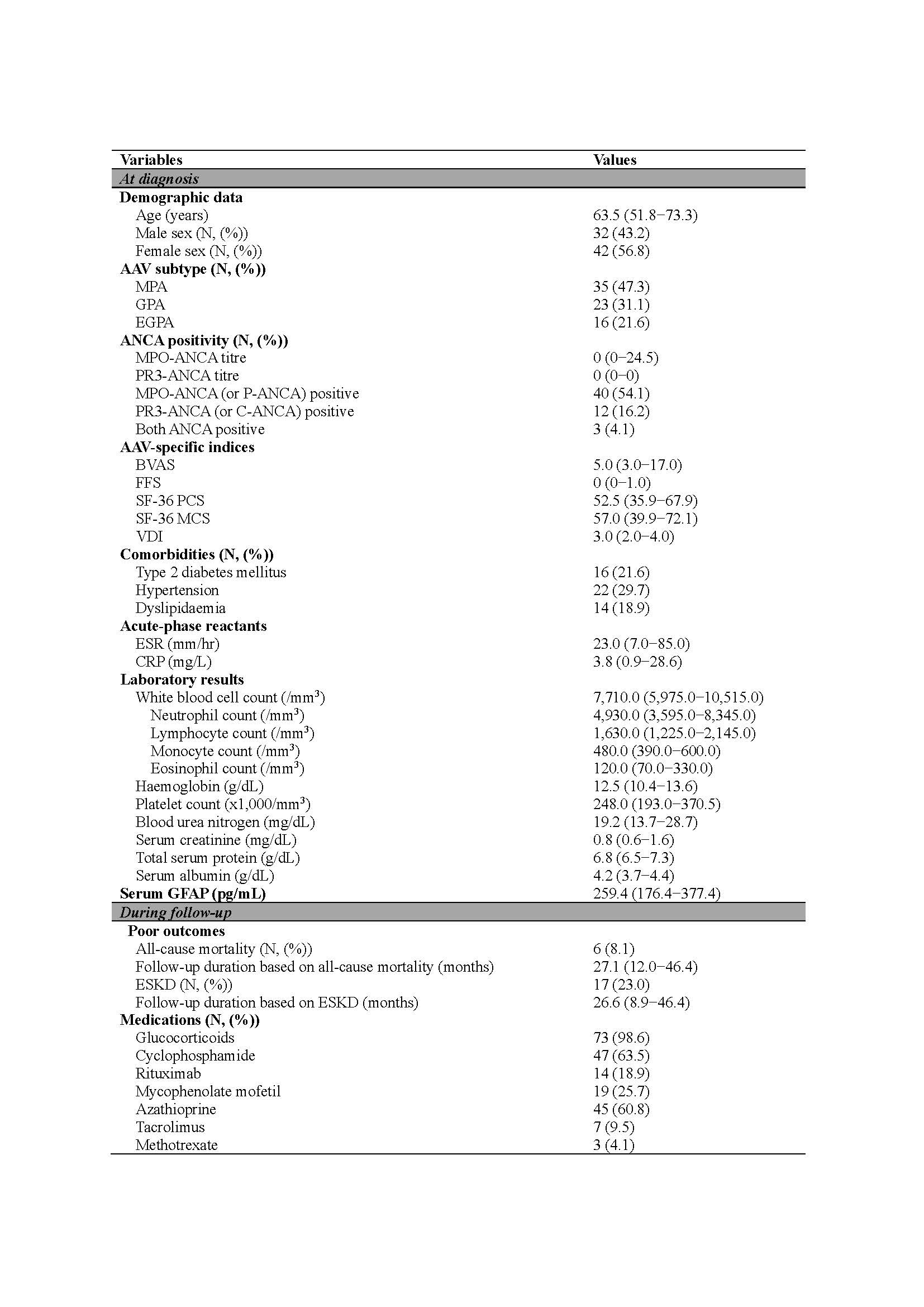
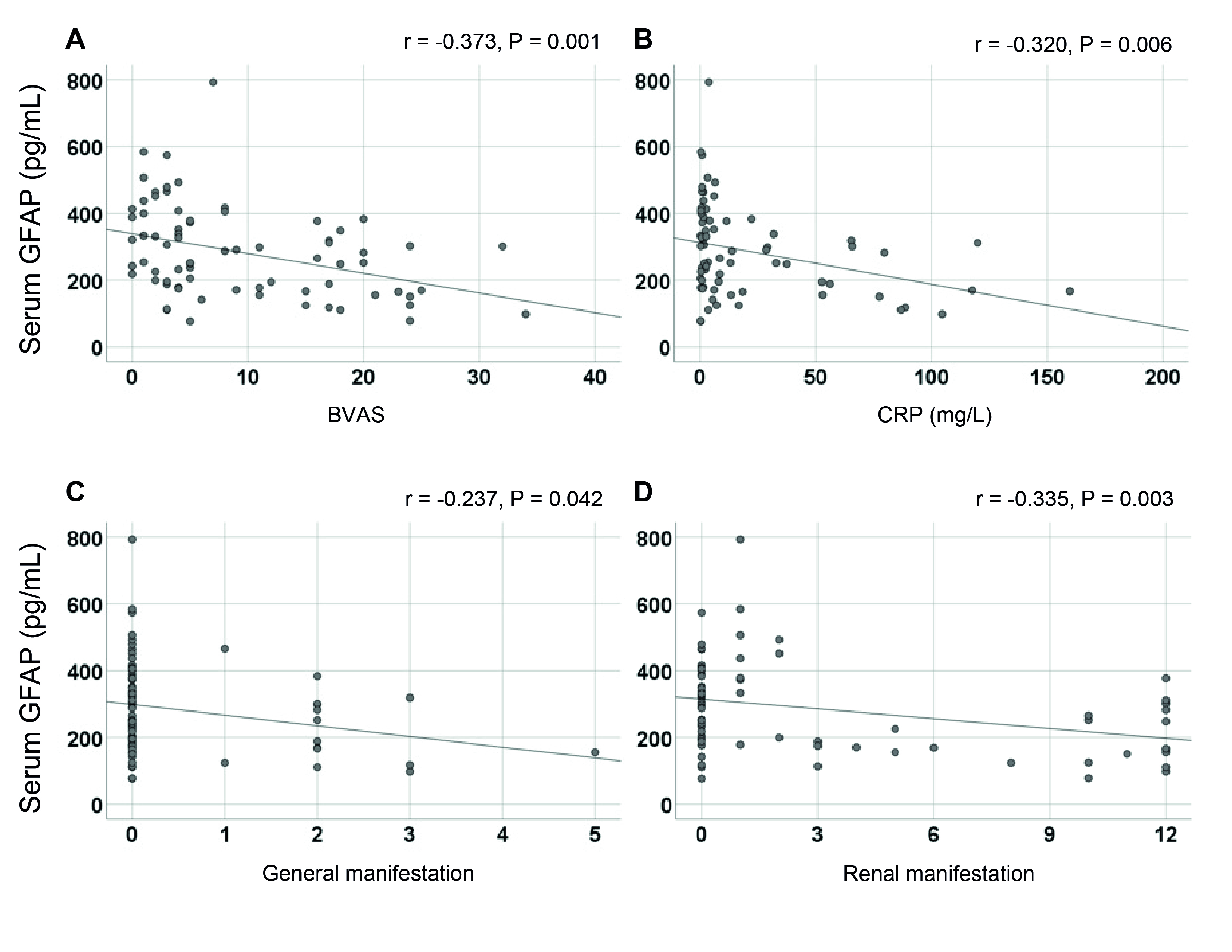
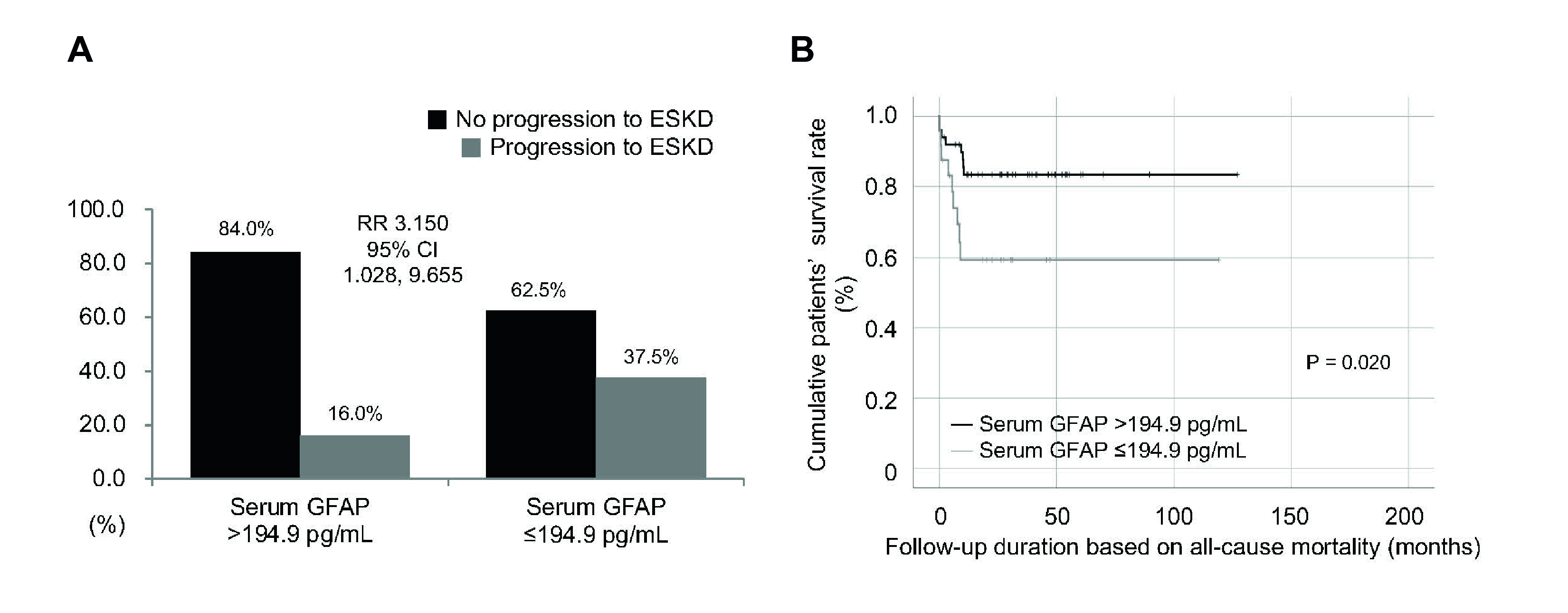
Results: At diagnosis, the median age of 74 patients was 63.5 years, with 32 males and 42 females. They were diagnosed with MPA (35), GPA (23), and EGPA (16). MPO-ANCA and PR3-ANCA were detected in 40 and 12 patients, respectively. Median BVAS, ESR, CRP, and serum GFAP were 5.0, 23.0 mm/h, 3.8 mg/L, and 259.4 pg/mL, respectively. During a median follow-up of 27.1 months, six patients (8.1%) died, and 17 (23.0%) progressed to ESKD over 26.6 months. Serum GFAP correlated significantly with BVAS (r = -0.373), CRP (r = -0.320), hemoglobin (r = 0.229), and serum albumin (r = 0.232). It was inversely associated with renal manifestations such as proteinuria (r = -0.409) and hematuria (r = -0.305). A serum GFAP ≤194.9 pg/mL at diagnosis was linked to a higher ESKD progression risk (RR 3.150). Patients with lower serum GFAP had reduced ESKD-free survival rates. However, GFAP did not predict all-cause mortality.
Conclusion: This study is the first to show that serum GFAP at diagnosis can estimate cross-sectional vasculitis activity by indicating renal involvement in patients with AAV. It also suggests that serum GFAP can partially predict progression to ESKD during follow-up. While further validation is needed, serum GFAP is proposed as a valuable complementary biomarker for newly diagnosed AAV patients, especially those with suspected renal involvement.
Values are expressed as a median (25~75 percentile) or N (%).
ANCA: antineutrophil cytoplasmic antibody; AAV: ANCA-associated vasculitis; MPA: microscopic polyangiitis; GPA: granulomatosis with polyangiitis; EGPA: eosinophilic granulomatosis with polyangiitis; MPO: myeloperoxidase; PR3: proteinase 3; P: perinuclear; C: cytoplasmic; BVAS: the Birmingham vasculitis activity score; FFS: the five-factor score; SF36: the 36-item short form survey; PCS: physical component summary; MCS: mental component summary; VDI: vasculitis damage index; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; GFAP: glial fibrillary acidic protein; ESKD: end-stage kidney disease.
Serum GFAP was significantly correlated with cross-sectional BVAS (A), CRP (B), and general (C) and renal (D) manifestations among nine BVAS systemic items.
GFAP: glial fibrillary acidic protein; BVAS: the Birmingham vasculitis activity score; CRP: C-reactive protein.
Compared to patients with serum GFAP >194.9 pg/mL, those with serum GFAP ≤194.9 pg/mL showed a higher risk for progression to ESKD (A) and a significantly lower cumulative ESKD-free survival rate (B).
RR: relative risk; ESKD: end-stage kidney disease; GFAP: glial fibrillary acidic protein.
To cite this abstract in AMA style:
Lee L, Yoon T, Park Y, Lee S. Serum Glial Fibrillary Acidic Protein Could Assess Cross-sectional Vasculitis Activity by Reflecting Renal Involvement in Patients with Antineutrophil Cytoplasmic Antibody-associated Vasculitis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/serum-glial-fibrillary-acidic-protein-could-assess-cross-sectional-vasculitis-activity-by-reflecting-renal-involvement-in-patients-with-antineutrophil-cytoplasmic-antibody-associated-vasculitis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-glial-fibrillary-acidic-protein-could-assess-cross-sectional-vasculitis-activity-by-reflecting-renal-involvement-in-patients-with-antineutrophil-cytoplasmic-antibody-associated-vasculitis/