Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: It has become clear that classification by phenotype is insufficient to explain the heterogeneity in clinical progression for many rheumatic diseases. Systemic sclerosis (SSc) has traditionally been categorized into limited or diffuse disease based on the extent of skin fibrosis. However, this classification system does not consistently predict which patients develop internal organ involvement. Gene expression can be used to categorize patients into four distinct “intrinsic subsets”: fibroproliferative, inflammatory, limited, and normal-like. We previously identified an association between the inflammatory subset and more severe skin disease, and the fibroproliferative subset and radiographic evidence of lung fibrosis. The objective of this study was to determine whether these intrinsic subsets could be used to predict longitudinal clinical outcomes over 3 years.
Methods: Patients with SSc (based on ACR/EULAR 2013 criteria) who had clinically active disease per the treating physician’s assessment were prospectively enrolled and underwent skin biopsies. Samples were analyzed to obtain gene expression data. Each patient was then assigned to an intrinsic subset using a GLMnet machine learning classifier. Clinical information including demographic, laboratory, body mass index (BMI), pulmonary function testing (PFT) and modified Rodnan skin score (mRSS) were collected at the time of skin biopsy and tracked over 3 years. Statistical analysis was used to determine whether these disease outcomes differed between intrinsic subsets at each timepoint. A total of 147 patients were included in this longitudinal analysis, out of the 165 enrolled in the baseline study.
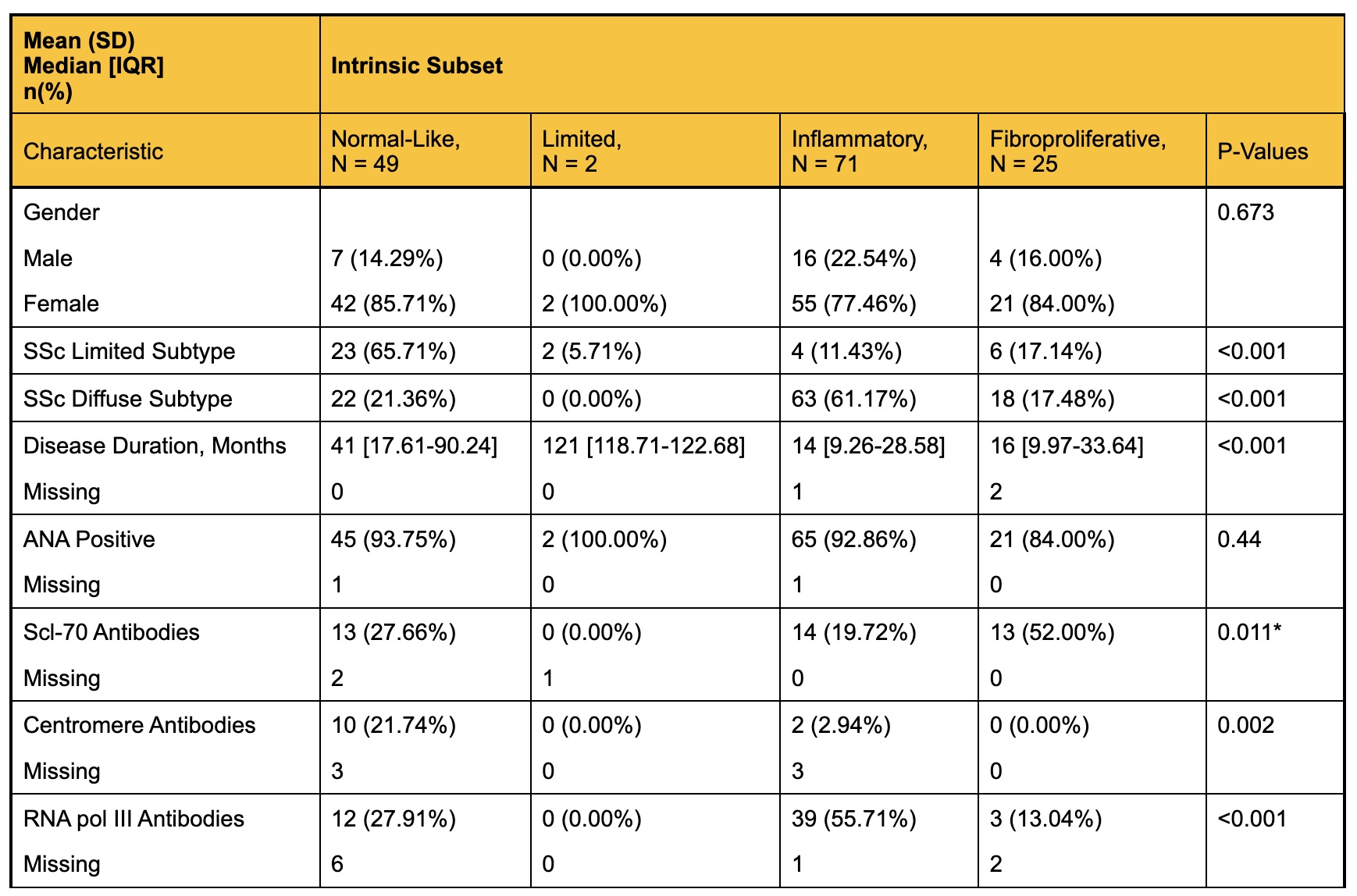
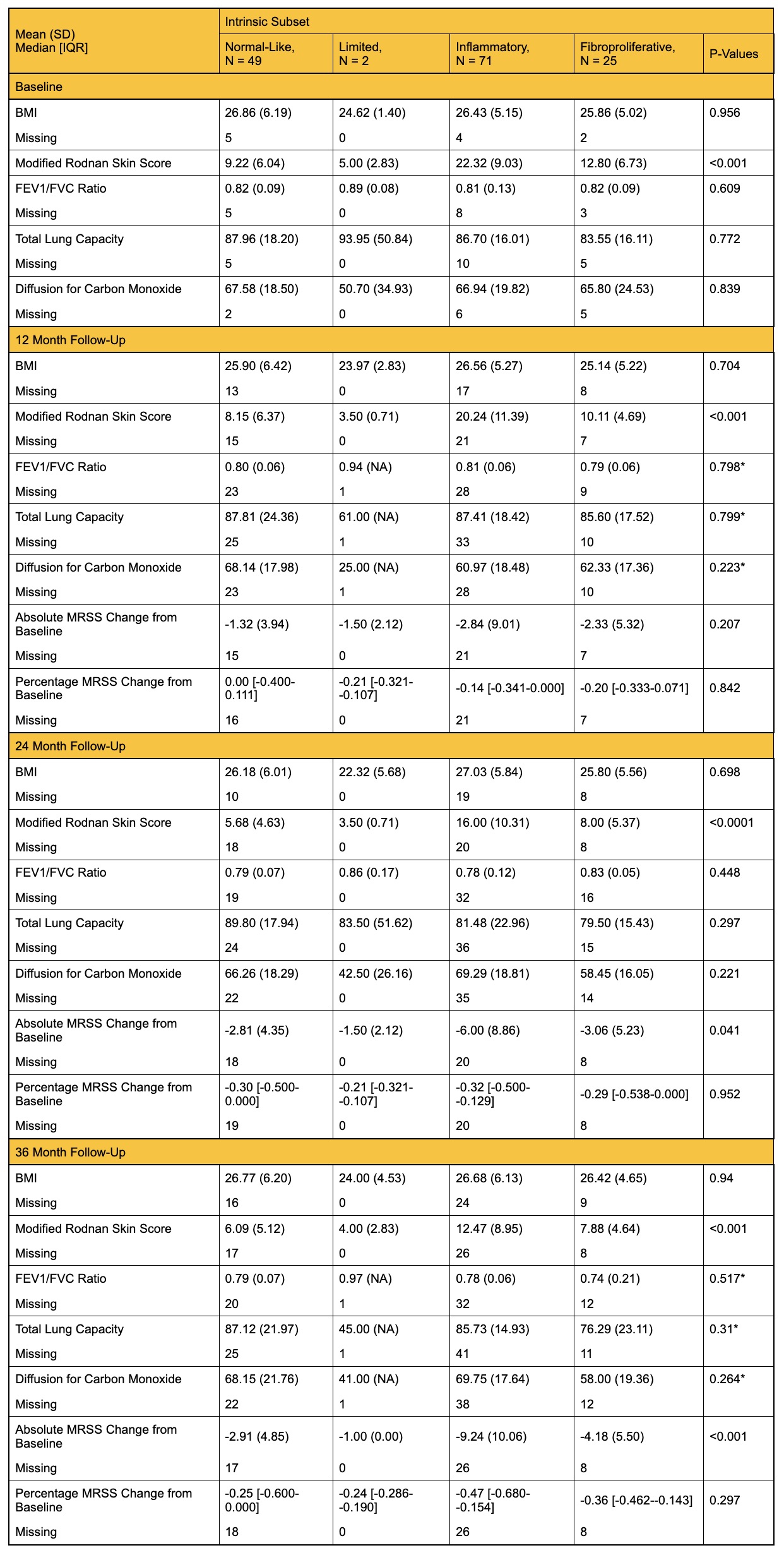
Results: Concordant with the baseline study, the normal-like subset was correlated with the limited cutaneous disease subtype and longer disease duration. Intrinsic subsets were also associated with specific autoantibodies (Table 1). Clinical disease outcomes stratified by intrinsic subset at each visit are shown in Table 2. The inflammatory subset consistently had the highest mRSS scores over 36 months, compared to other subsets. This subset also showed the most improvement in skin score by 36 months, with an average absolute change of -9.24 (p< 0.001). The fibroproliferative subset had lower average diffusion capacity (DLCO) compared to the normal-like and inflammatory subsets at the 36-month timepoint, although this difference was not statistically significant. There were no differences in BMI between intrinsic subsets at any timepoint.
Conclusion: This study demonstrates that gene expression signatures in the skin of SSc patients correlate with clinical disease characteristics over time. The inflammatory subset had more severe skin disease even 3 years after initial skin biopsy but had the most dramatic improvement in skin score. Patients in the fibroproliferative subset, who had evidence of more radiographic lung fibrosis at baseline, demonstrated a trend toward reduced DLCO by 3 years, suggesting development of clinical interstitial lung disease (ILD). These findings imply that molecular signatures in the skin can predict longitudinal disease outcomes in patients with systemic sclerosis.
To cite this abstract in AMA style:
Field N, Yang M, Gupta N, Shramuk M, Muhammad L, Goh V, Espinoza M, Yuan Y, Parvizi R, Aren K, Carns M, Goldberg I, Chung L, Khanna D, McMahan Z, Whitfield M, Hinchcliff M. Molecular Signatures in the Skin as Predictors of Longitudinal Clinical Trajectories in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/molecular-signatures-in-the-skin-as-predictors-of-longitudinal-clinical-trajectories-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/molecular-signatures-in-the-skin-as-predictors-of-longitudinal-clinical-trajectories-in-patients-with-systemic-sclerosis/