Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Cardiac involvement in Systemic Sclerosis (SSc) is widely recognized as heterogeneous and, when clinically evident, it is associated with a poor prognosis. Recently, five cardiac magnetic resonance (CMR) phenotypes in SSc have been identified (Knight DS et al. European Heart Journal 2023). These phenotypes do not align with the existing clinical subgroup classifications or autoantibody statuses, yet each has a distinct 5-year prognosis. Our objective is to test the long-term prognostic significance of this classification system in an external cohort and to compare ECG Holter monitor parameters, NT-proBNP, and troponin T levels across these groups.
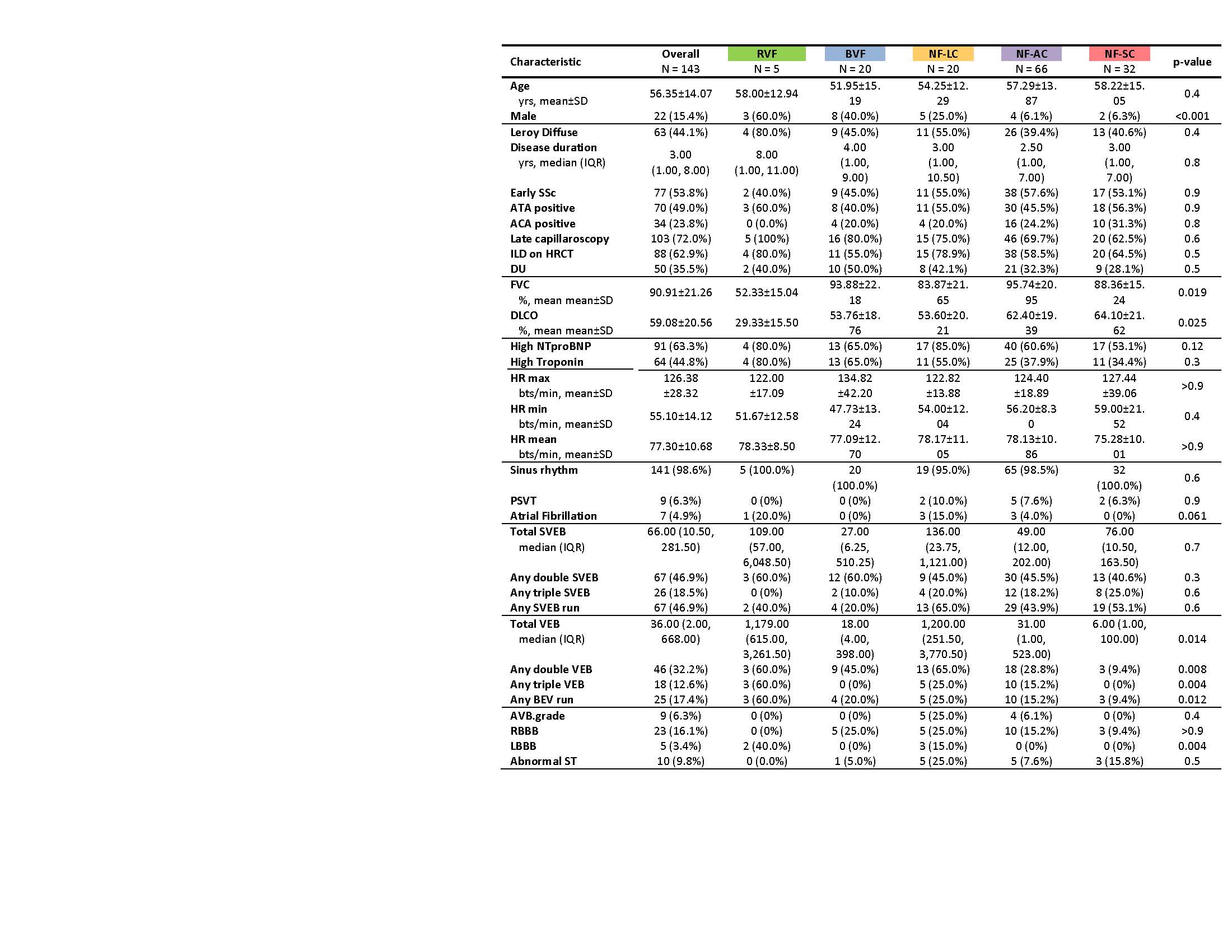
Methods: CMR assessments were conducted in three Italian tertiary centers on consecutive SSc patients who presented symptoms of dyspnoea, palpitations, or chest pain. Based on the CMR findings, patients were categorized into five distinct groups: those with dilated right hearts with right ventricular failure (RVF); biventricular failure with dilatation and dysfunction (BVF); and those with normal function, categorized further based on cavity sizes as average cavity (NF-AC), small cavity (NF-SC), and large cavity (NF-LC). The study focused on comparing clinical characteristics, serum troponin and NT-proBNP levels, ECG Holter monitor parameters, and 10-year survival outcomes across these groups.
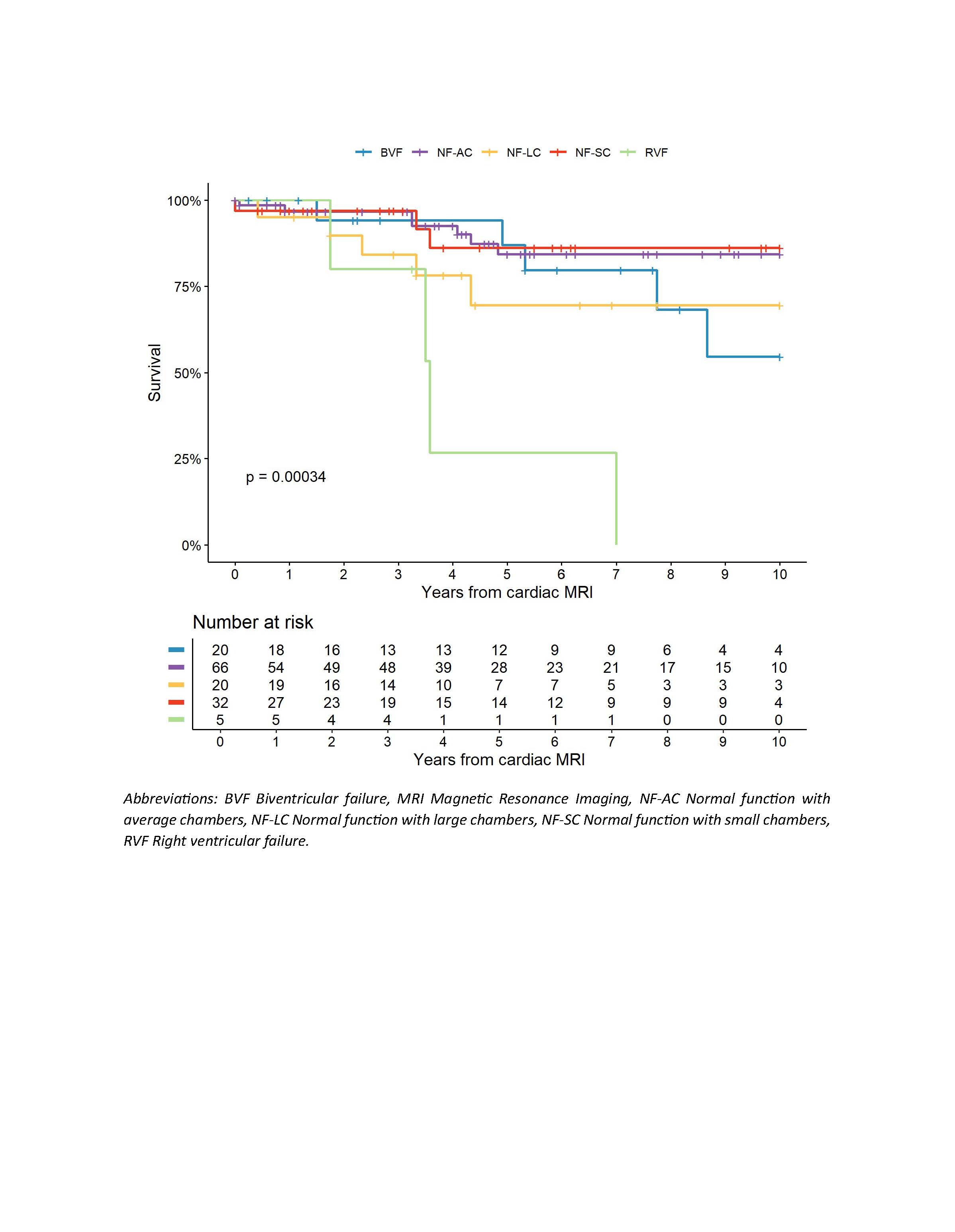
Results: Table 1 presents the clinical characteristics and assessed parameters of the 143 enrolled patients across the CMR subsets. The distributions for NF-AC, NF-SC, NF-LC, BVF, and RVF were 46.2%, 22.4%, 14.0%, 14.0%, and 3.5%, respectively. Proportions of male patients and pulmonary function tests showed statistically significant differences across the subsets. Troponin T and NT-proBNP values were similar across all subsets. The NF-LC and RVF groups exhibited Left Bundle Branch Block (LBB) more frequently and more ventricular ectopic beats (VEB) compared to other groups. There was a variation in 10-year survival rates across the groups, with patients in the RVF, NF-LC, and BVF categories showing poorer prognosis (Figure 1).
Conclusion: This data confirms the prognostic value of the proposed CMR subsets in an another European SSc cohort, highlighting that subsets with poorer prognosis are associated with a higher arrhythmic burden.
To cite this abstract in AMA style:
Bosello S, De Lorenzis E, De Luca G, Tonutti A, Batani v, Cerasuolo P, Natalello G, Lanzo L, Alonzi G, Fiore S, Di Murro S, Zoli A, Boni V, Marano R, Gabrielli F, Del Galdo F, Knight D, Muthurangu V, Denton C, De Santis M, Matucci Cerinic M, D'Agostino M. Arrhythmic Burden, Myocardial Markers, and Long-term Survival in Distinct Cardiac Magnetic Resonance Subsets of Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/arrhythmic-burden-myocardial-markers-and-long-term-survival-in-distinct-cardiac-magnetic-resonance-subsets-of-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/arrhythmic-burden-myocardial-markers-and-long-term-survival-in-distinct-cardiac-magnetic-resonance-subsets-of-systemic-sclerosis/