Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Hospitalizations due to systemic lupus erythematosus (SLE) often stem from lupus flares and infections. Socioeconomic factors influencing outcomes in SLE hospitalizations have been studied at various levels, showing that increasing age, lack of insurance, and non-white race worsen outcomes. Conflicting results exist on the effect of poverty on mortality. Analyzing recent national database data is crucial for targeted interventions to improve patient outcomes. This study analyzed the National Readmission Database (NRD) from 2016 to 2019, examining how income, insurance status, and patient location impacted length of stay, mortality, and total charges, along with a review of prior studies.
Methods: We analyzed SLE-related hospital discharges from non-elective admissions using NRD data from 2016 to 2019. Hospitalizations were identified using ICD code M32. Excluding cases with missing data and pediatric patients, outcomes were defined as length of stay (LOS), all-cause mortality, and total charges. Income levels were categorized as less than $64,000 or more, and insurance status was classified as insured (Medicaid, Medicare, Private insurance) or uninsured (No insurance, No charge). Patient location was classified as metro or non-metro. Age, number of diagnoses, and procedures performed were covariates. Similar regression analysis were performed for a superset of all patients and compared with the SLE subset.
Results:
Year-over-Year Trends in Lupus-Related Hospitalizations
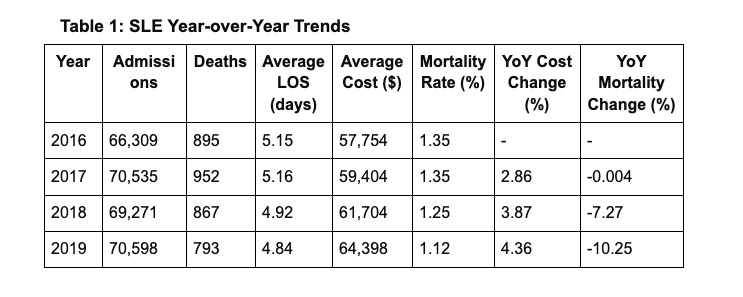
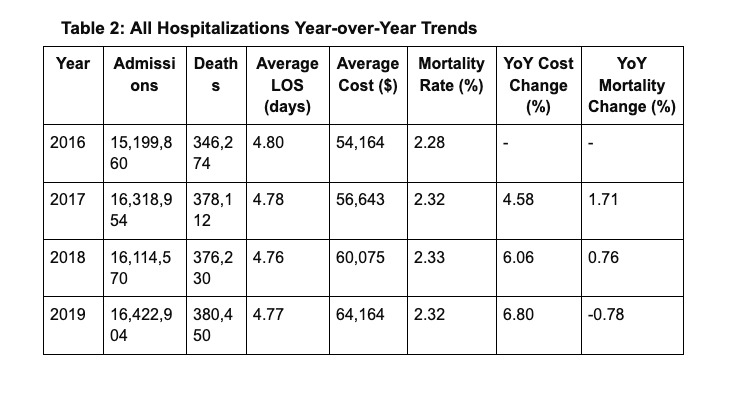
From 2016 to 2019, SLE hospital admissions increased from 66,309 to 70,598, while the mortality rate decreased from 1.35% to 1.12%. The average LOS decreased from 5.15 to 4.84 days, and average cost per hospitalization increased from $57,754 to $64,398. Overall hospital admissions increased from 15,199,860 to 16,422,904, with costs rising from $54,164 to $64,164. The mortality rate peaked at 2.33% in 2018 before decreasing to 2.32% in 2019. SLE hospitalizations consistently incurred higher costs but had lower mortality rates compared to overall data.
Multivariate Analysis for Lupus-Related Admissions
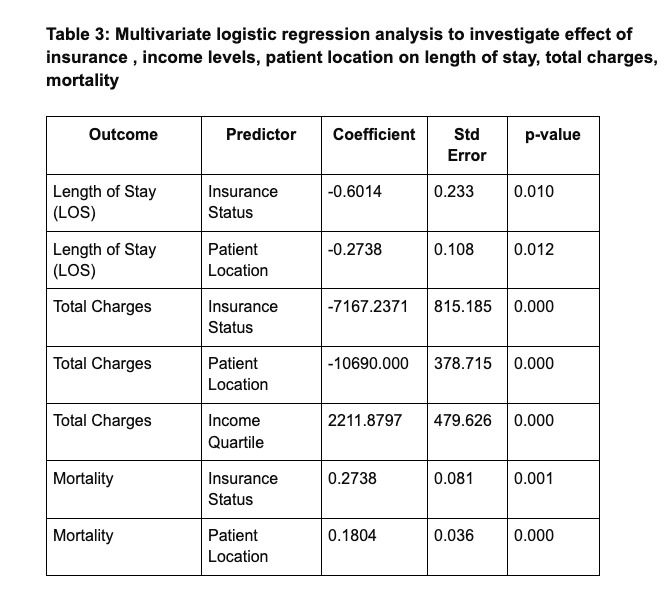
LOS: No insurance and non-metro locations were linked to shorter LOS, while age increased LOS.
Total Charges: No insurance and non-metro locations were linked to lower charges, while higher income and age increased charges.
Mortality: No insurance and non-metro locations increased mortality risk, as did higher age.
Conclusion: The NRD analysis from 2016 to 2019 highlights the socioeconomic determinants of SLE hospitalization outcomes. Patients without insurance and those in non-metro areas tend to have shorter LOS and incur lower costs but face higher mortality rates. These findings underscore the importance of socioeconomic factors in SLE patient outcomes. Targeted interventions, such as improving insurance coverage and healthcare access in non-metro areas, could enhance patient outcomes and reduce healthcare disparities.
To cite this abstract in AMA style:
Arya P V A, Rondla M, Tirupur Ponnusamy J, C Unnikrishnan D. Socioeconomic Determinants of Lupus Hospitalization Outcomes: A Review of Current Knowledge and Analysis of the 2016-2019 NRD Database [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/socioeconomic-determinants-of-lupus-hospitalization-outcomes-a-review-of-current-knowledge-and-analysis-of-the-2016-2019-nrd-database/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/socioeconomic-determinants-of-lupus-hospitalization-outcomes-a-review-of-current-knowledge-and-analysis-of-the-2016-2019-nrd-database/