Session Information
Date: Saturday, November 16, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Spondyloarthritis (SpA) is a heterogeneous group of inflammatory arthritides that includes ankylosing spondylitis (AS), psoriatic arthritis (PsA), enteropathic-related arthritis, reactive arthritis, and undifferentiated SpA. To date, there are no studies evaluating the coexistence of SpA with Raynaud’s Phenomenon (RP), morphea, or personal or family history (FH) of systemic sclerosis (SSc). Overlap between these conditions has been limited to case reports. This study aims to determine the prevalence of SpA among individuals with RP, morphea, or personal or FH of SSc, and to identify any distinct characteristics that may distinguish this subgroup of patients.
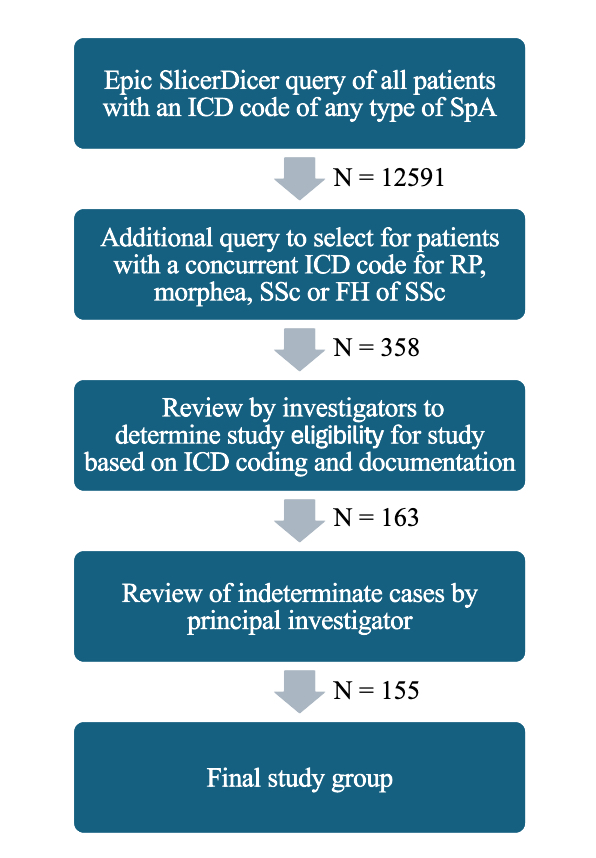
Methods: The study utilized the electronic health record (EHR) database of Houston Methodist Hospital to identify patients diagnosed with SpA that were concurrently diagnosed with RP, morphea, SSc or FH of SSc. The query was based on the presence of relevant International Classification of Diseases (ICD) codes. Investigators assessed patient charts to confirm eligibility through documentation and the presence of diagnosis codes. Data was collected on patient demographics, SpA diagnosis, presence of RP, morphea, SSc, FH of SSc, HLA-B27 status or other HLA-B type, and the presence of other autoantibodies.
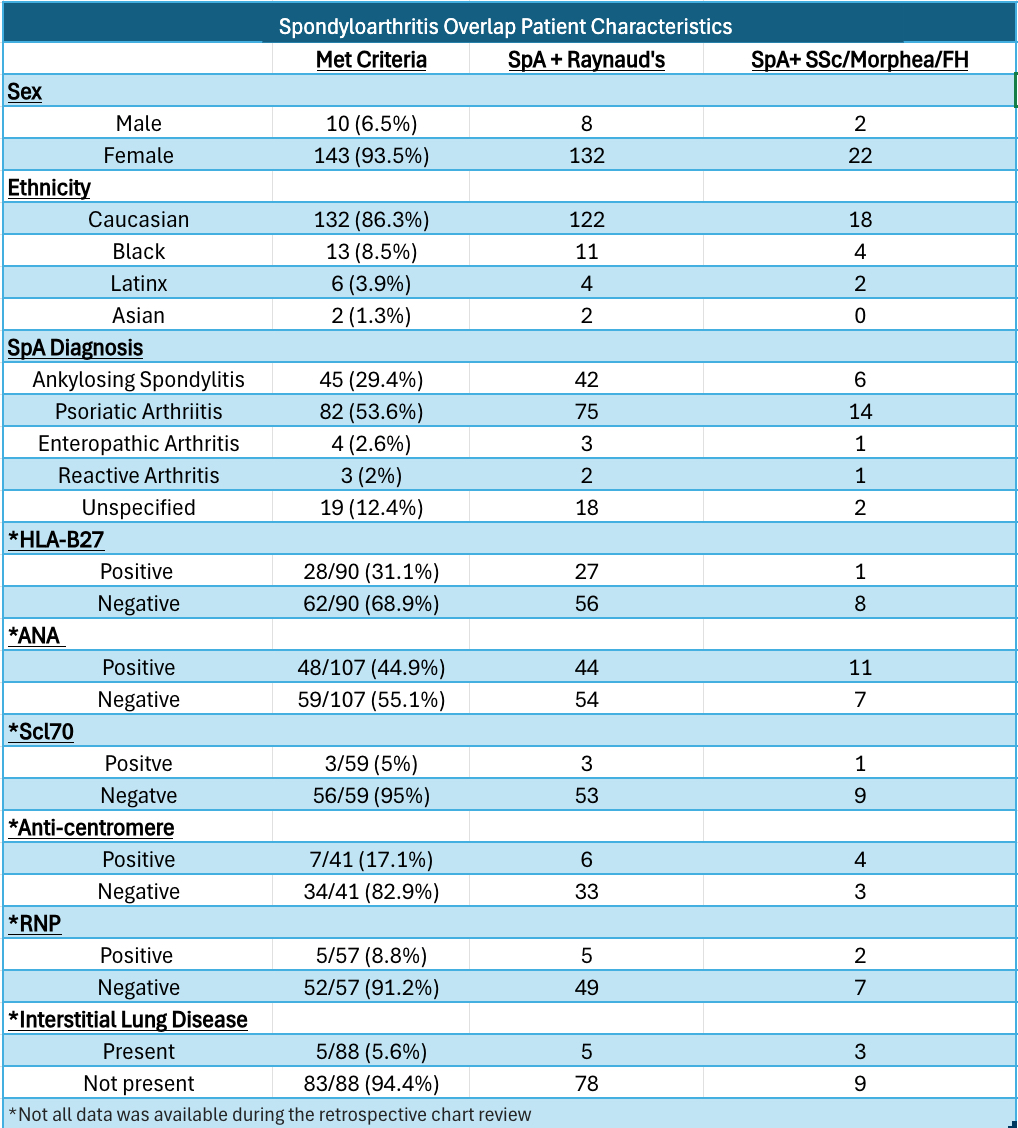
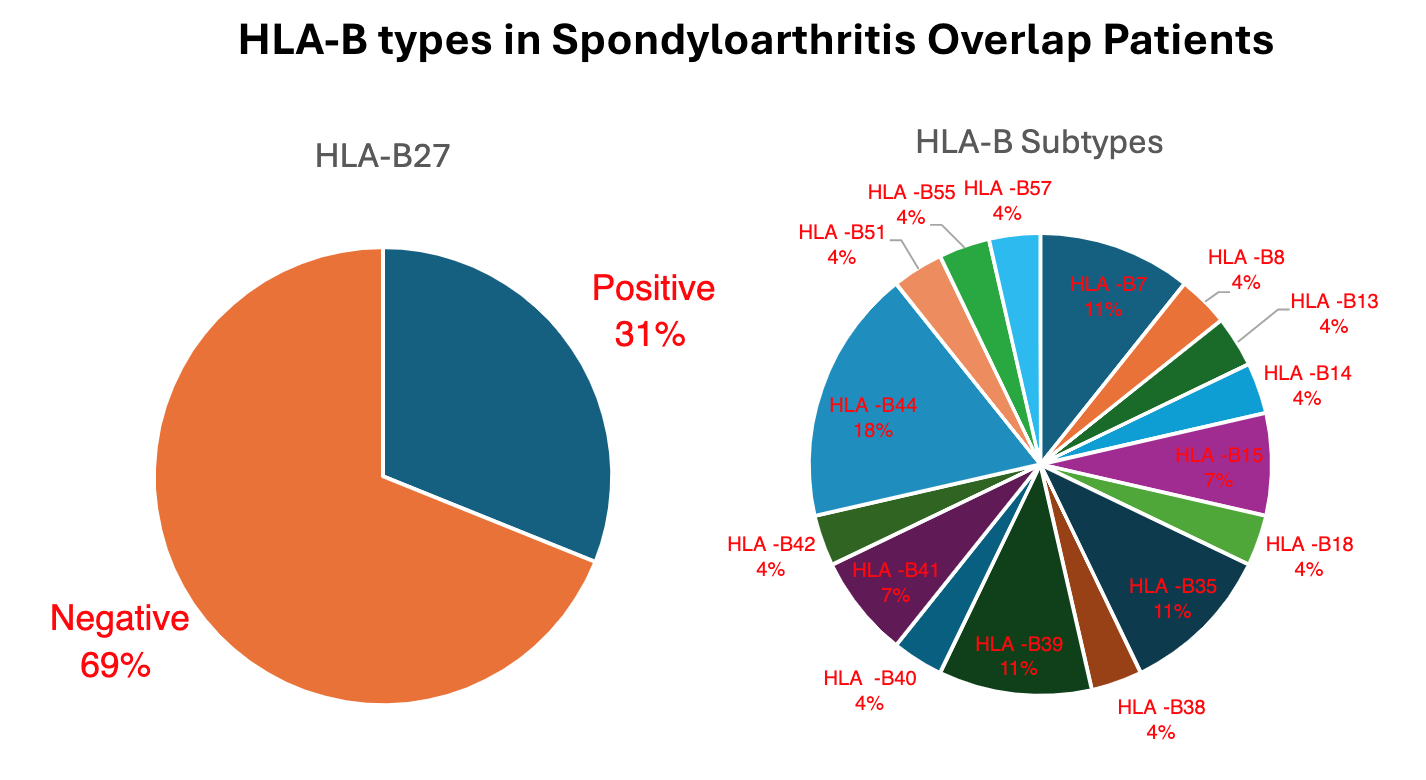
Results: The initial EHR query revealed 358 patients with an ICD-10 code of SpA and either RP, morphea, SSc or FH of SSc. Investigators determined that 153 patients met criteria after thorough chart review. 91.5% of patients had SpA with RP (n=140). 15.7% of patients had SpA with morphea, SSc or a FH of SSc (n=24). The majority of patients were female (93.5%, n=143). Caucasian was the most prevalent ethnicity (86.3%, n=132). Notably, PsA was the most frequently associated SpA diagnosis (53.6%, n=82). Of patients with available data, 68.9% (62/90) were HLA-B27 negative. 15 of these patients had HLA-B subtyping available; the most frequent subtypes were HLA-B44, HLA-B35, and HLA-B7. Although data was limited, we found that 44.9% (48/107) patients with SpA overlap as defined in our study had a positive anti-nuclear antibody (ANA) and 17.1% (7/41) had positive anti-centromere antibodies.
Conclusion: This study highlights the presence of RP, morphea, and SSc in patients with SpA, a finding previously limited to case reports. The majority of affected patients are Caucasian females with a negative HLA-B27 status, suggesting a potentially distinct phenotype of SpA characterized by concurrent RP, morphea, or SSc. These findings may prompt consideration for diagnostic and therapeutic approaches, necessitating further investigation such as HLA-typing and assessment of treatment response. “MHC-I (major histocompatibility complex class I)-opathy” has emerged as a new term describing a family of inflammatory conditions with overlapping clinical manifestations and a strong genetic link to the MHC-I antigen presenting pathway. Overlap typically includes features of SpA, psoriasis, Behcet’s disease, inflammatory bowel disease and uveitis. Future studies can investigate if RP, morphea or SSc should be included as part of “MHC-I-opathy.”
Legend: ICD = Internal Classification of Disease, SpA = spondyloarthritis, SSC = systemic sclerosis, RP = Raynaud’s phenomenon
Legend: SpA = Spondyloarthritis, ANA= Anti-Nuclear antibodies, Scl-70 = Anti-Topoisomerase I antibodies, RNP = Anti-Ribonucleoprotein antibodies
To cite this abstract in AMA style:
Dev A, Roy C, Jagannath D, Cloutet A, Kazzaz S. Coexistence of Raynaud’s Phenomenon, Morphea or Scleroderma in Spondyloarthritis Patients: Insights from a Retrospective Cohort Study Highlighting a Unique Phenotype [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/coexistence-of-raynauds-phenomenon-morphea-or-scleroderma-in-spondyloarthritis-patients-insights-from-a-retrospective-cohort-study-highlighting-a-unique-phenotype/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/coexistence-of-raynauds-phenomenon-morphea-or-scleroderma-in-spondyloarthritis-patients-insights-from-a-retrospective-cohort-study-highlighting-a-unique-phenotype/