Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is among the most significant extra-articular manifestations of rheumatoid arthritis (RA), clinically affecting 8-15% of RA patients, and accounting for approximately 6% of all RA deaths. While anti-citrullinated protein antibodies (ACPAs) and rheumatoid factor (RF) are associated with prevalent RA-ILD, their role in predisposing to RA-ILD onset is not well established, particularly for ACPA subtypes and RF isotypes. The purpose of this study was to investigate ACPA subtypes and RF isotypes as predictors of prevalent and incident RA-ILD.
Methods: Within a large, multicenter prospective cohort of U.S. Veterans with RA, we performed a cross-sectional study of prevalent RA-ILD and a cohort study of incident RA-ILD. RA-ILD diagnoses were systematically captured with an informatics-based screening approach and validated by a board-certified rheumatologist through standardized medical record review of clinical diagnoses, chest imaging, and pathology. Individuals with prevalent RA-ILD (diagnosed before enrollment) were excluded from incident analyses. Concentrations of RF isotypes (IgA, IgM, IgG) and ACPA subtypes (n=18 ACPAs) were measured via ELISA or a multiplex bead-based assay, respectively, using serum from enrollment then log-transformed and standardized. Multivariable logistic (prevalent RA-ILD) and Cox (incident RA-ILD) regression models were used to evaluate the individual associations of RF/ACPAs with RA-ILD adjusting for age, sex, race, and smoking status. Additional models adjusted for commercial anti-CCP antibody positivity to evaluate additive prediction.
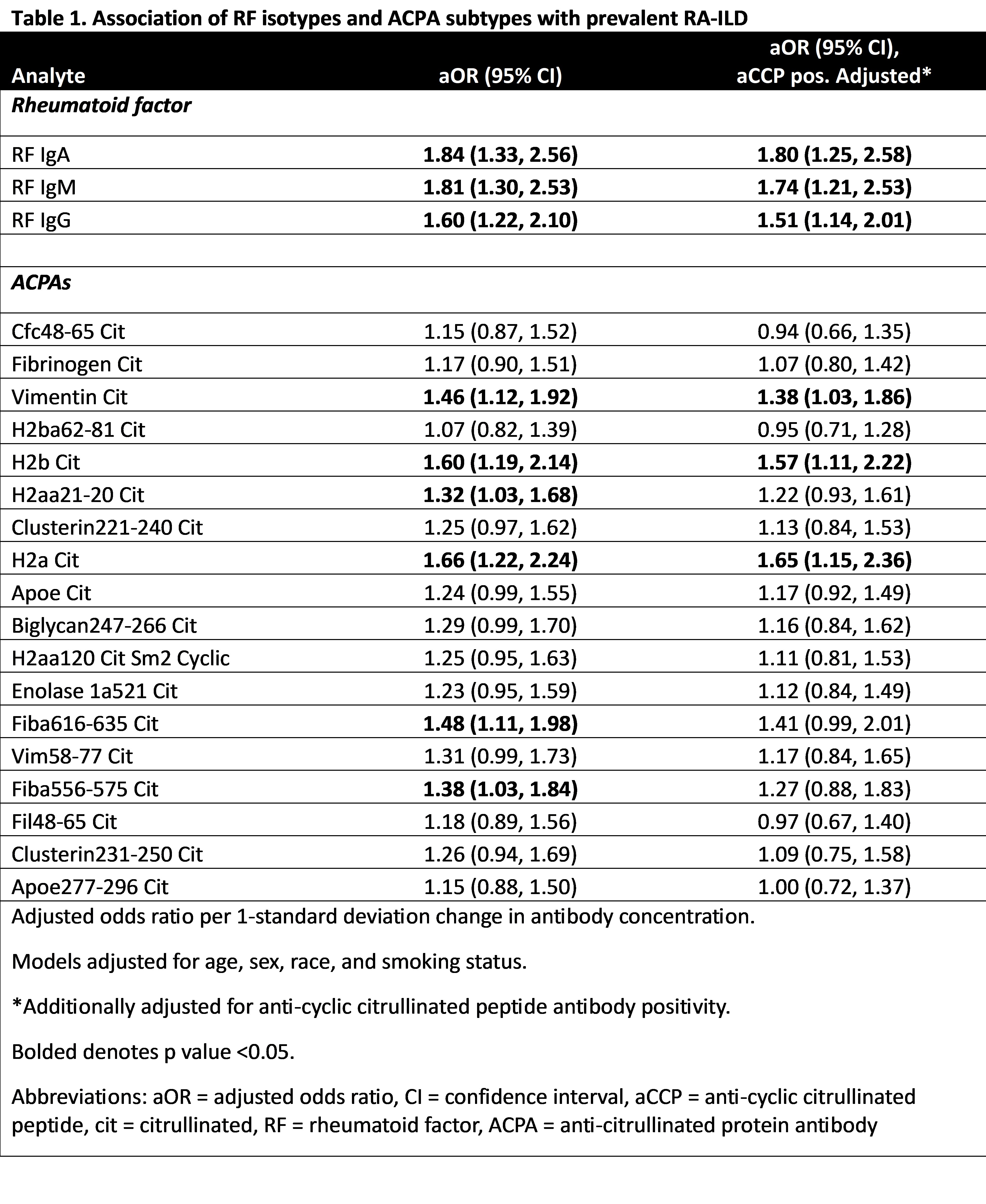
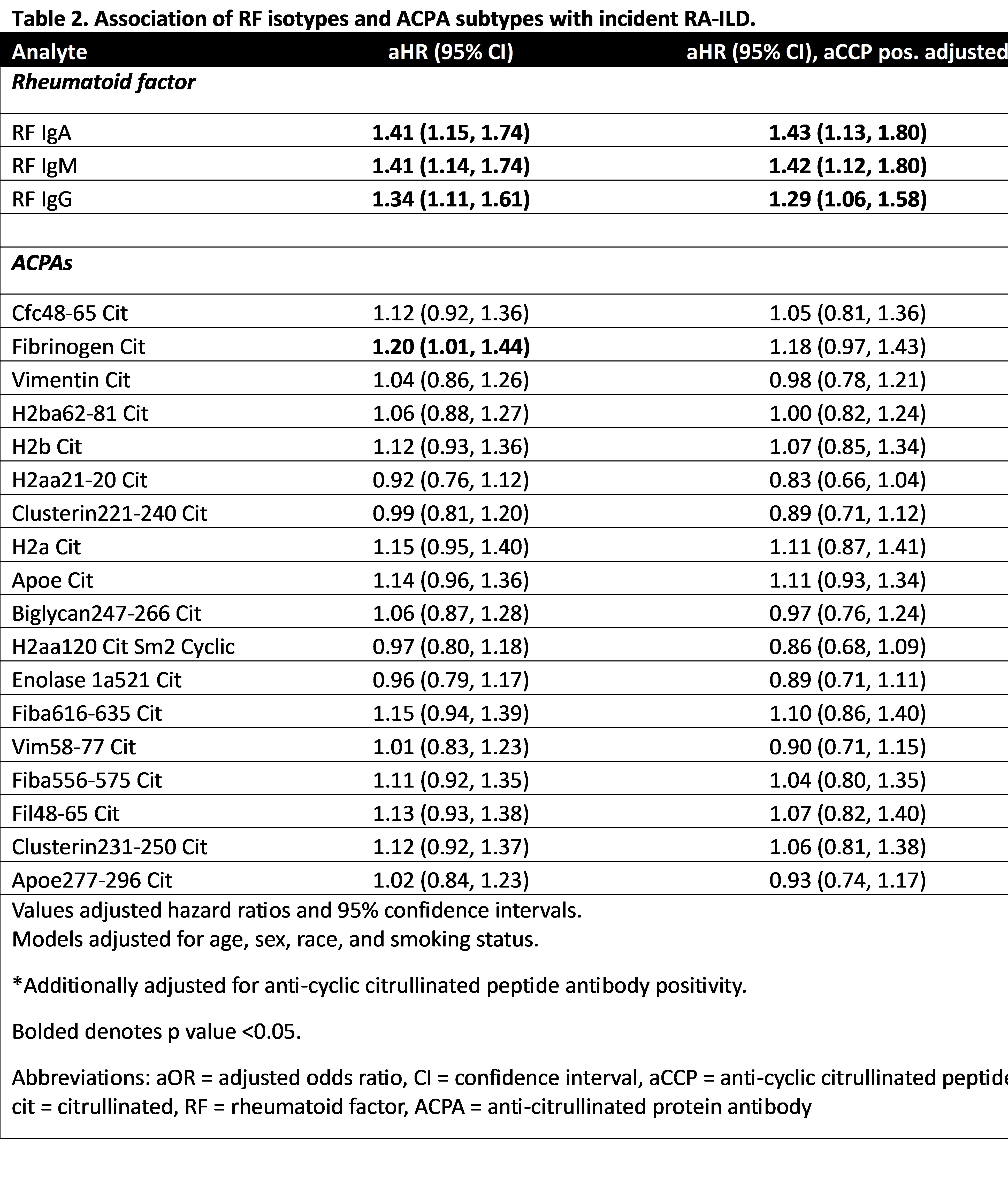
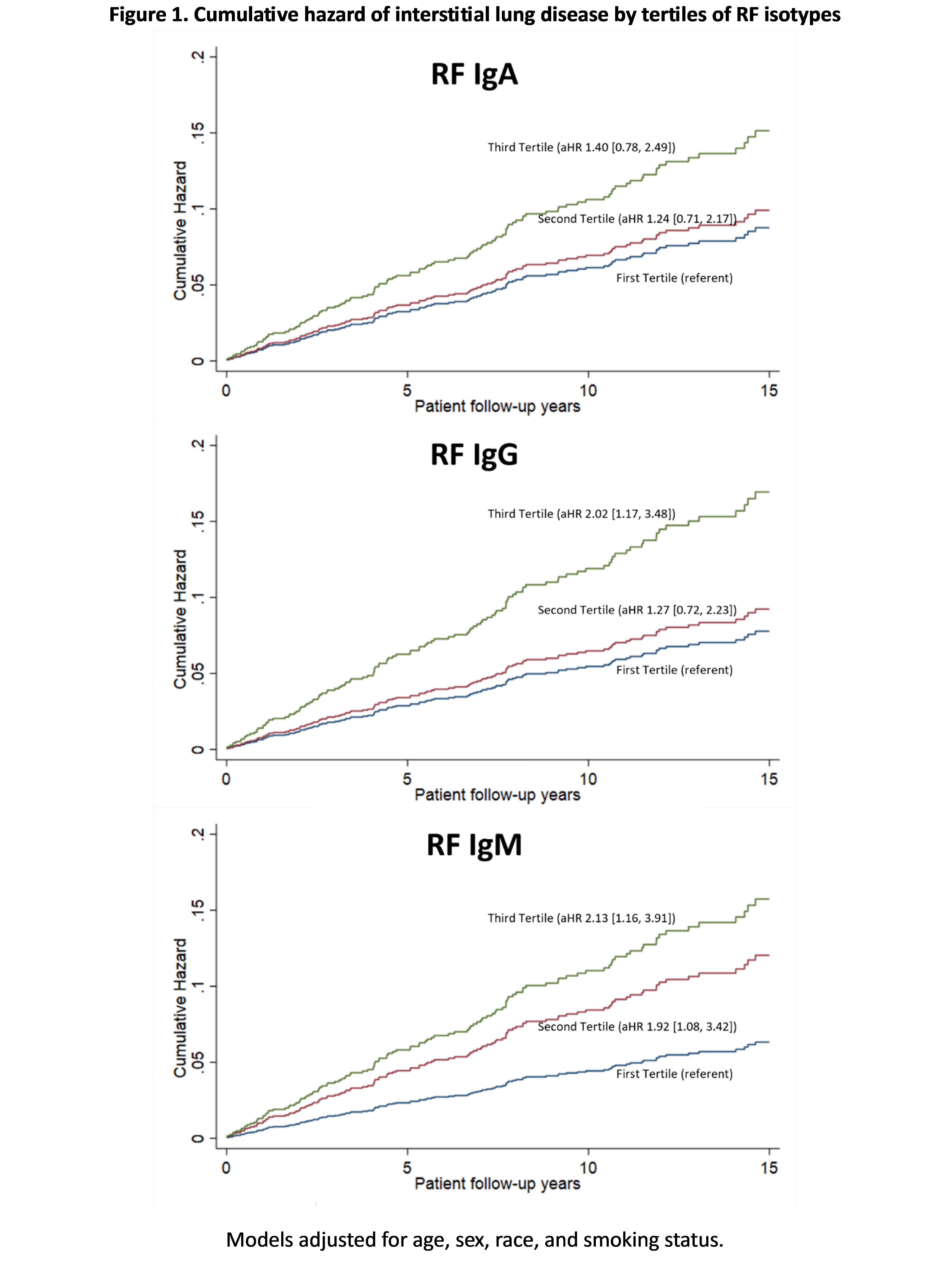
Results: Among 1666 participants with RF isotypes (mean age 63.5 years, 90.7% male), 66 had prevalent RA-ILD while 122 developed incident RA-ILD. Characteristics were similar among participants with ACPA subtypes where 58 of 1,458 participants had prevalent RA-ILD, and 108 developed incident RA-ILD. Higher concentrations of IgA (aOR per 1 SD 1.84, 1.33-2.56), IgM (aOR 1.81, 1.30-2.53), and IgG (aOR 1.60, 1.22-2.10) RF were associated with prevalent RA-ILD (Table 1). Six of eighteen ACPA subtypes were significantly associated with prevalent RA-ILD, with three remaining associated independent of commercial anti-CCP positivity (vimentin cit, h2b cit, h2a cit). Higher concentrations of IgA (aHR 1.41, 1.15-1.74), IgM (aHR 1.41, 1.14-1.74) and IgG (aHR 1.34, 1.11-1.61) RF were also significantly associated with incident RA-ILD (Table 2). Among ACPAs, only anti-cit-fibrinogen was associated with incident RA-ILD, which did not persist after adjustment for commercial anti-CCP positivity. RA patients with the highest values of IgA, IgM, and IgG RF isotypes had a 1.4 to >2-fold higher risk of developing incident ILD (tertile 3 vs. tertile 1, Figure 1).
Conclusion: RF isotypes, particularly IgA and IgM, are more closely associated with prevalent and incident RA-ILD in RA than ACPA subtypes. RF antibodies may precede clinical disease, and measurement of RF isotypes may aid in risk stratification for incident RA-ILD.
To cite this abstract in AMA style:
Welch J, Yang Y, Baker J, Wysham K, Ascherman D, Monach P, Kerr G, Reimold A, Cannon g, Kunkel G, Robinson W, Duryee M, Thiele G, Mikuls T, England B. ACPA Subtypes, RF Isotypes, and the Risk of Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/acpa-subtypes-rf-isotypes-and-the-risk-of-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/acpa-subtypes-rf-isotypes-and-the-risk-of-rheumatoid-arthritis-associated-interstitial-lung-disease/