Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Recent evidence has linked abnormal body weight, underweight or obesity, with poor disease outcomes in adults with inflammatory arthritis. Yet, little is known about potential similar associations in children with JIA. Therefore, we investigated the association between BMI categories and time to start treatments and attain disease outcomes in children with JIA.
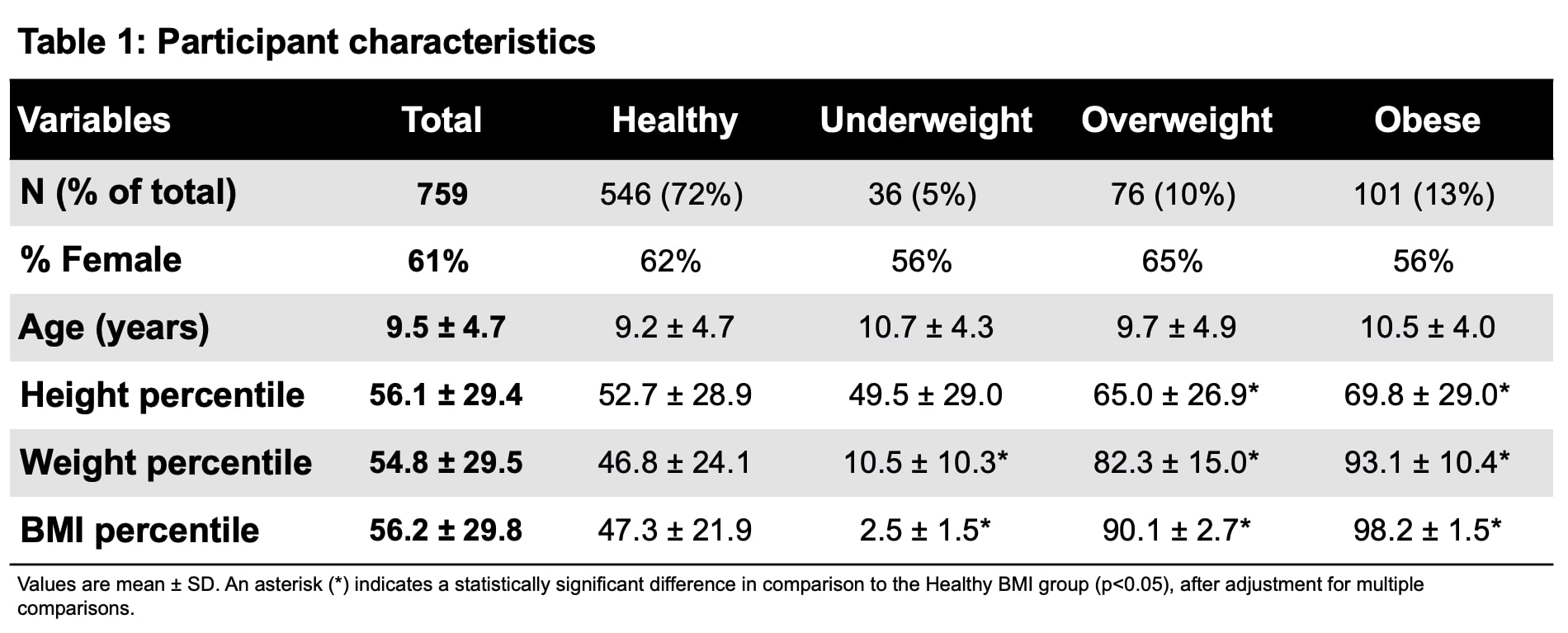
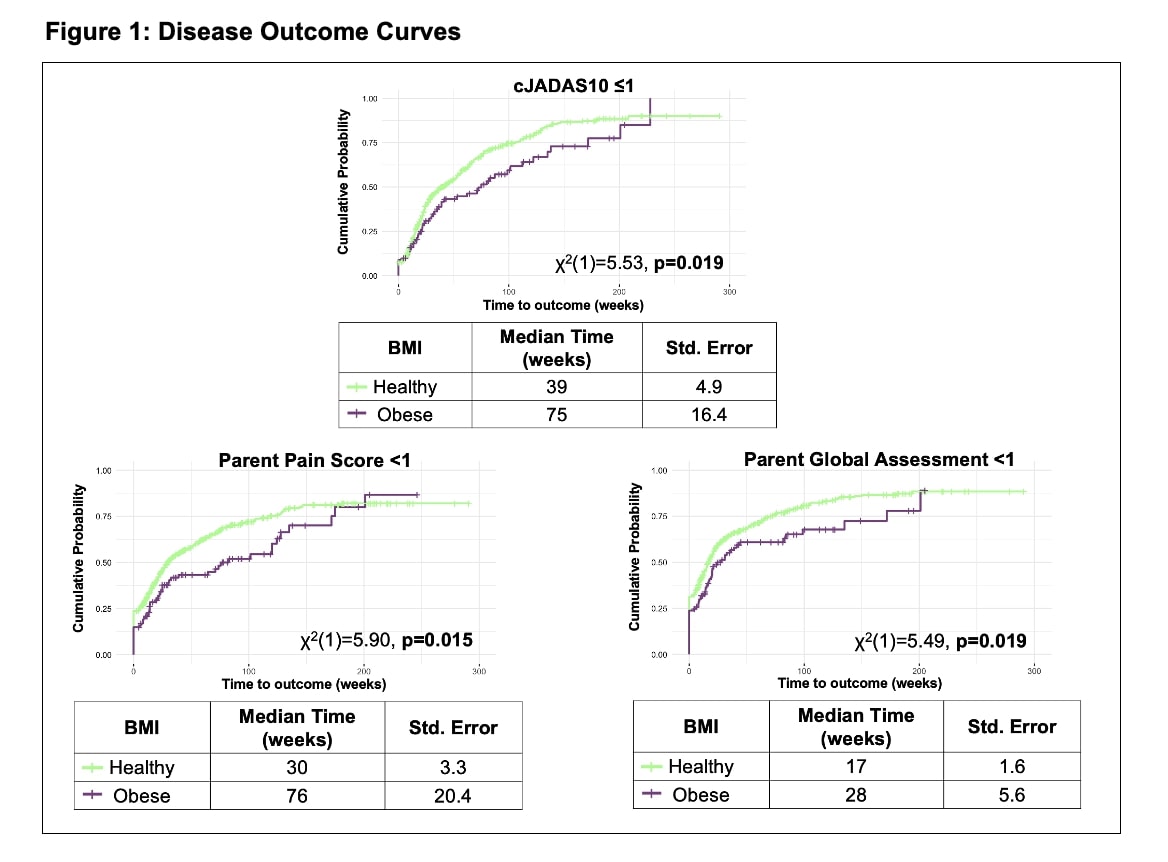
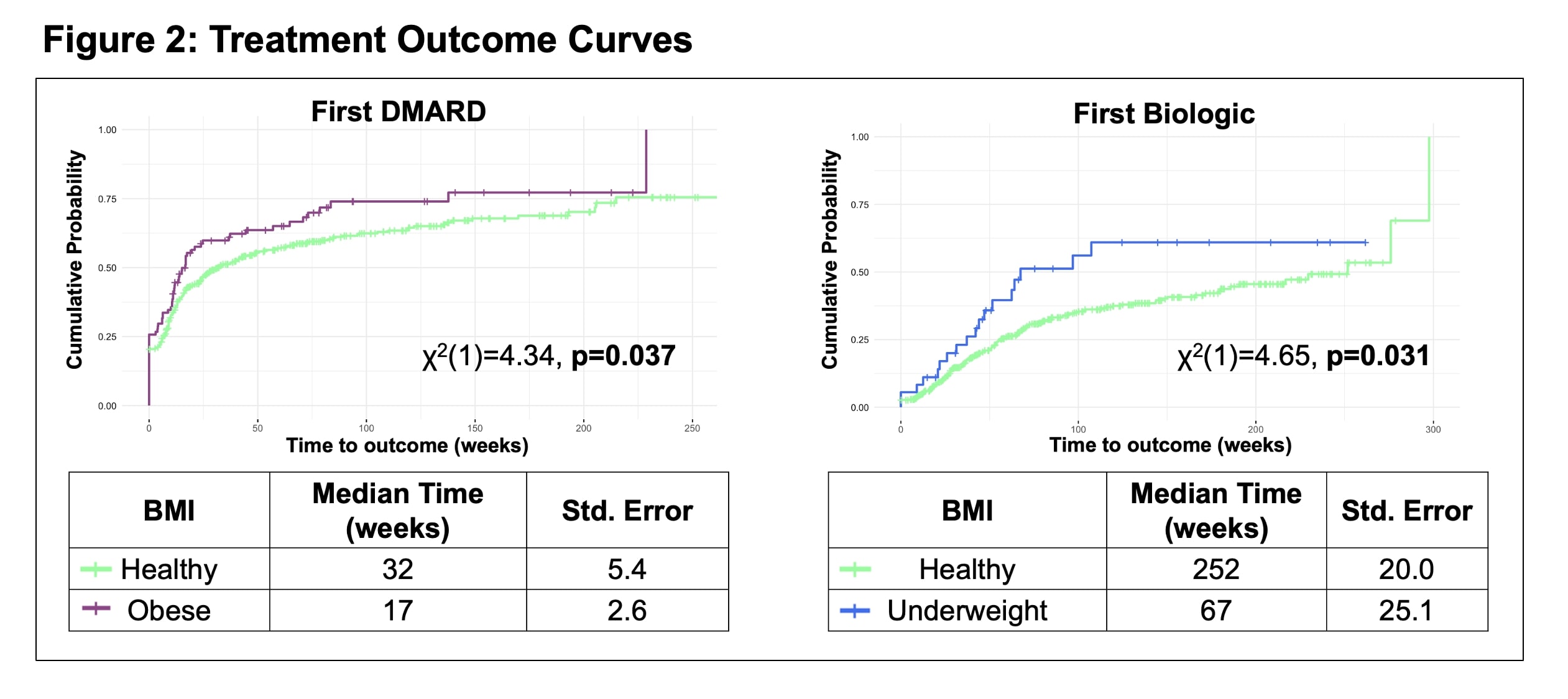
Methods: Data were captured prospectively through the Canadian Alliance of Pediatric Rheumatology Investigators (CAPRI) JIA Registry. This national research registry follows newly diagnosed patients with JIA and collects data at each clinic visit. Based on age, sex, height, and weight at enrolment, BMI was categorized for each patient as underweight (< 5th percentile), healthy (5th to < 85th percentile), overweight (85th to < 95 th percentile), or obese (≥95th percentile) according to the WHO growth charts. For each BMI category, Kaplan–Meier curves examined time to clinical Juvenile Arthritis Disease Activity Score 10 (cJADAS10) ≤1, pain score (parent and patient reported) < 1, quality of life (patient reported) >9, parent global assessment < 1, physician global assessment < 1, and active joint count < 1. For these disease outcomes, shorter times are considered optimal. Time to start treatments included conventional DMARD, biologic DMARD, joint injections, and systemic corticosteroids. Log-rank tests compared outcomes across BMI categories; healthy weight served as the reference category.
Results: We included 759 patients enrolled in the Registry between February 2017 and May 2023 (61% female; mean±SD age 9.5±4.7 years); majority of patients had a healthy BMI (Table 1). The obese group took significantly longer to attain cJADAS10 ≤1 (χ2(1)=5.53, p=0.019, median difference in time to reach outcomes compared to reference category [MD]=36 weeks), parent pain score < 1 (χ2(1)=5.90, p=0.015, MD=46 weeks), and parent global assessment < 1 (χ2(1)=5.49, p=0.019, MD=11 weeks) (Figure 1). Time to first DMARD was significantly shorter in obese patients (χ2(1)=4.34, p=0.037, MD=15 weeks), and time to first biologic was significantly shorter in underweight patients (χ2(1)=4.65, p=0.031, MD=185 weeks) (Figure 2). No other treatments or outcomes were significantly different between BMI categories.
Conclusion: Children with JIA in the obese group took longer to attain disease control based on both clinical and parent-reported outcomes compared to those with healthy BMI, despite earlier treatment escalation to DMARDs. Additionally, those who were underweight also required earlier treatment escalation to biologics. Further analyses will explore weight percentile groups, covariates including ethnicity and JIA subtype, and changes in body composition overtime. Altogether, these findings may help inform clinicians on anticipated treatment responses and disease outcomes when educating and counseling families about body composition.
To cite this abstract in AMA style:
Morin S, BEATTIE K, Bolaria R, Cellucci T, Chedeville G, Chhabra A, Dancey P, Gerschman T, Heale L, Herrington J, Huber A, Jariwala M, Proulx-Gauthier J, Rumsey D, Schmeling H, Guzman J, Batthish M. The Association Between Body Composition and Disease and Treatment Outcomes in Patients with Juvenile Idiopathic Arthritis: Results from the CAPRI Registry [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-association-between-body-composition-and-disease-and-treatment-outcomes-in-patients-with-juvenile-idiopathic-arthritis-results-from-the-capri-registry/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-body-composition-and-disease-and-treatment-outcomes-in-patients-with-juvenile-idiopathic-arthritis-results-from-the-capri-registry/