Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Hypertension accounts for >54% of modifiable cardiovascular disease (CVD) risk and although 49% of US outpatient visits occur in specialty clinics, only 10% of these visits recommend follow-up for high blood pressure (BP). In 2014, BP Connect was created to systematically address high BP in specialty clinics by adapting evidence-based staff protocols from primary care (PC) settings. We previously published that across 28,000 visits in three rheumatology clinics, BP Connect cut rates of high BP visits in half and doubled timely PC follow-up. BP Connect has been replicated in community clinics and maintained in three academic rheumatology clinics for over seven years. The aim of this study was to assess BP Connect’s scalability in diverse rheumatology clinics and feasibility in non-rheumatology specialties.
Methods: We examined rates of PC follow-up of high BP among patients in two gynecology clinics and two urban rheumatology clinics pre and post BP Connect implementation. Our primary analysis compares time to PC follow-up pre and post implementation. All adult patients with high clinic BP were protocol-eligible post 2021 implementation (vs pre 2019).
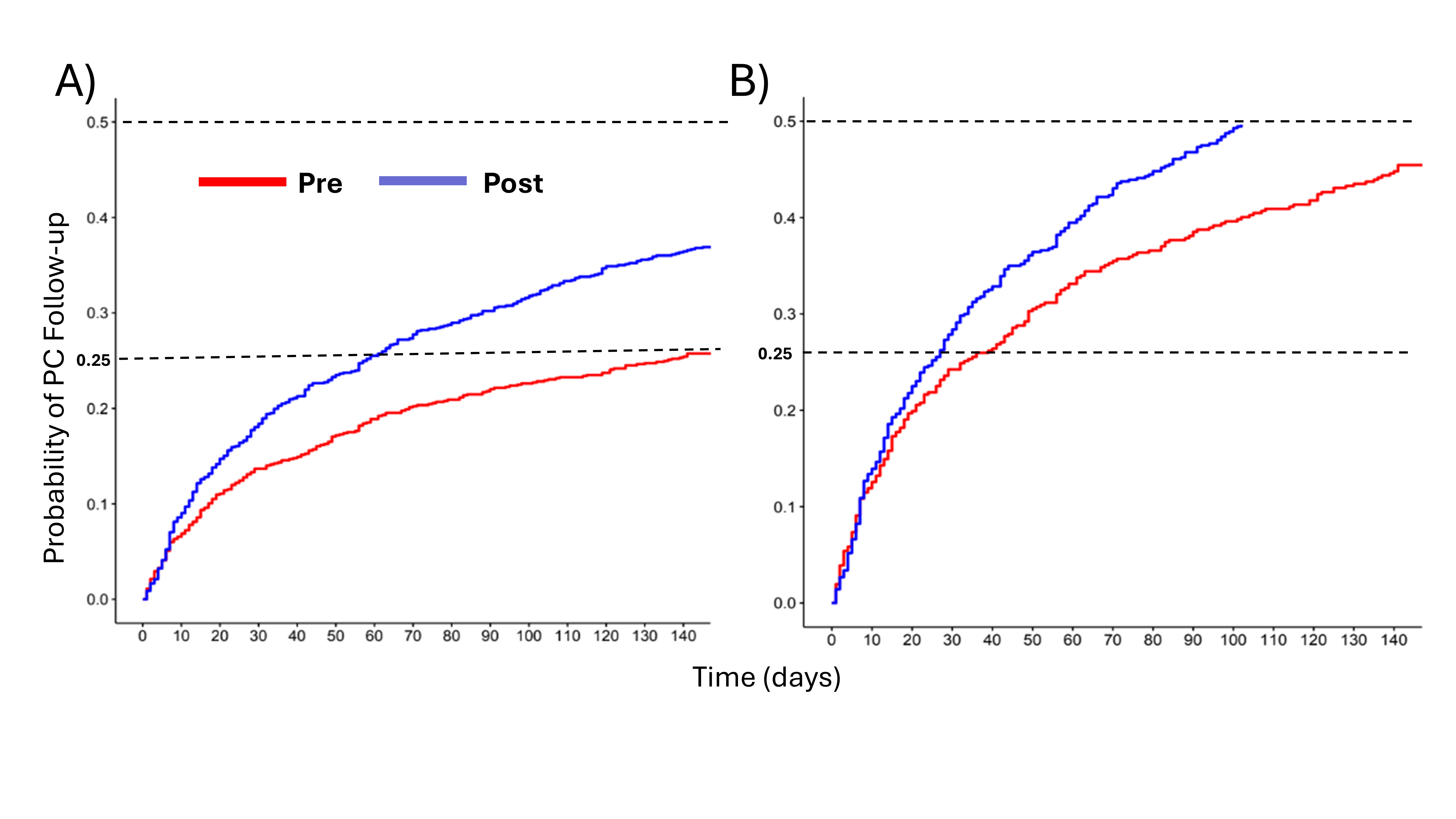
BP Connect’s EHR prompts clinical staff (medical assistants, nurses and schedulers) to: Check, re-measuring high BP ( >/=140/90), Advise CVD risk and Connect patients to PC follow-up within 1 month using automated EHR orders (avg < 4 min). BP rechecks indicated intention to treat (ITT) post-protocol. The gynecologic clinics had no prior protocol for high BP follow-up. The rheumatology clinics had a prior institutional hypertension protocol with EHR remeasurement prompts and asynchronous referrals to PCP. The BP Connect implementation protocol included clinic staff engagement, education, EHR reminder alerts with order sets, performance feedback with numerical data, and real time PC follow-up orders and scheduling. The Kaplan-Meier figures compare time to PC follow-up pre/post. Sociodemographics collected from EHR data were included in multivariable Cox models (HR, 95% CI).
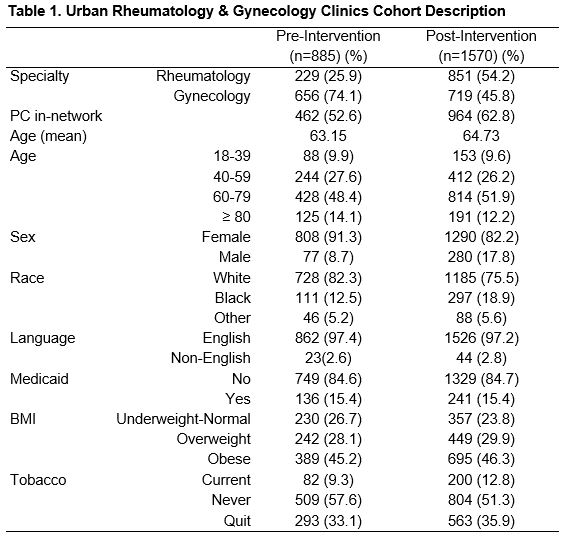
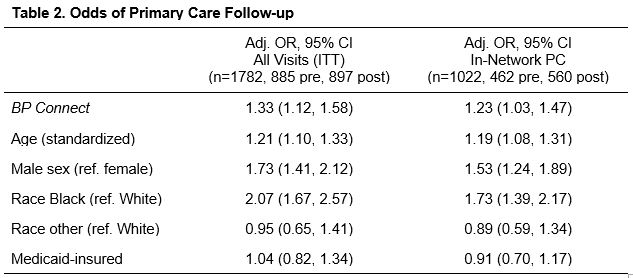
Results: We analyzed 885 eligible pre-protocol visits and 1570 eligible post-protocol visits across the four clinics. Table 1 shows the pre/post cohorts were evenly matched. Overall, 27.1% pre-protocol followed-up vs 38.6% post (ITT, p< 0.0001); limiting to those with in-network PC 47.6% pre vs 60% post (p< 0.0001). Time to 25% follow-up with PC was 78 days faster for visits after vs before BP Connect implementation (pre 136 days, post 58, see Figure 1A). Fig 1B restricts to in-network PC where 50% follow-up is achievable post-protocol but never pre-protocol. Patients of Black race [aOR 2.07 (1.67, 2.57)] and men [aOR 1.73 (1.41, 2.12)] were among those more likely to improve follow-up (Table 2, ITT). Relationships were similar when restricting to in-network PC (Table 2, In-Network).
Conclusion: Findings indicate that BP Connect intervention results in primary care follow-up over two months sooner. This was observed in both urban rheumatology and gynecology/non-rheumatology clinics, supporting generalizability. Reduced racial disparities were also observed.
To cite this abstract in AMA style:
Figueroa Baiges A, Gazeley D, Messina M, Hanlon B, Ramly E, Rosenthal A, Stewart L, Williams M, Brown H, Bartels C. BP Connect Improves Follow-up of High Blood Pressure in Urban Rheumatology and Non-Rheumatology Clinics [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/bp-connect-improves-follow-up-of-high-blood-pressure-in-urban-rheumatology-and-non-rheumatology-clinics/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bp-connect-improves-follow-up-of-high-blood-pressure-in-urban-rheumatology-and-non-rheumatology-clinics/