Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: While often preventable, falls are a common, costly, and serious outcome in the U.S. population: more than one in four adults ³65 years old fall each year, with an estimated $50 billion in costs per year. While many individuals with SLE of all ages share risk factors for falls with older adults, little is known about the burden of falls in this population. We aimed to characterize the prevalence and correlates of falls in a population-based cohort of adults with SLE.
Methods: Participants were recruited from an ongoing, population-based cohort of individuals with validated SLE [Georgians Organized Against Lupus (GOAL)] for a single study visit (10/2019-5/2022), during which they reported their falls (including number of falls and injuries requiring medical attention) over the past year, as well as the factors they associated with their fall(s), both intrinsic (within the individual, e.g., impaired mobility) and extrinsic (outside the individual, e.g., environmental hazards). Descriptive statistics were calculated, and age-, sex-, and race-adjusted associations [adjusted odds ratios (aORs)] of various sociodemographic and clinical characteristics with falls were assessed with multivariable logistic regression.
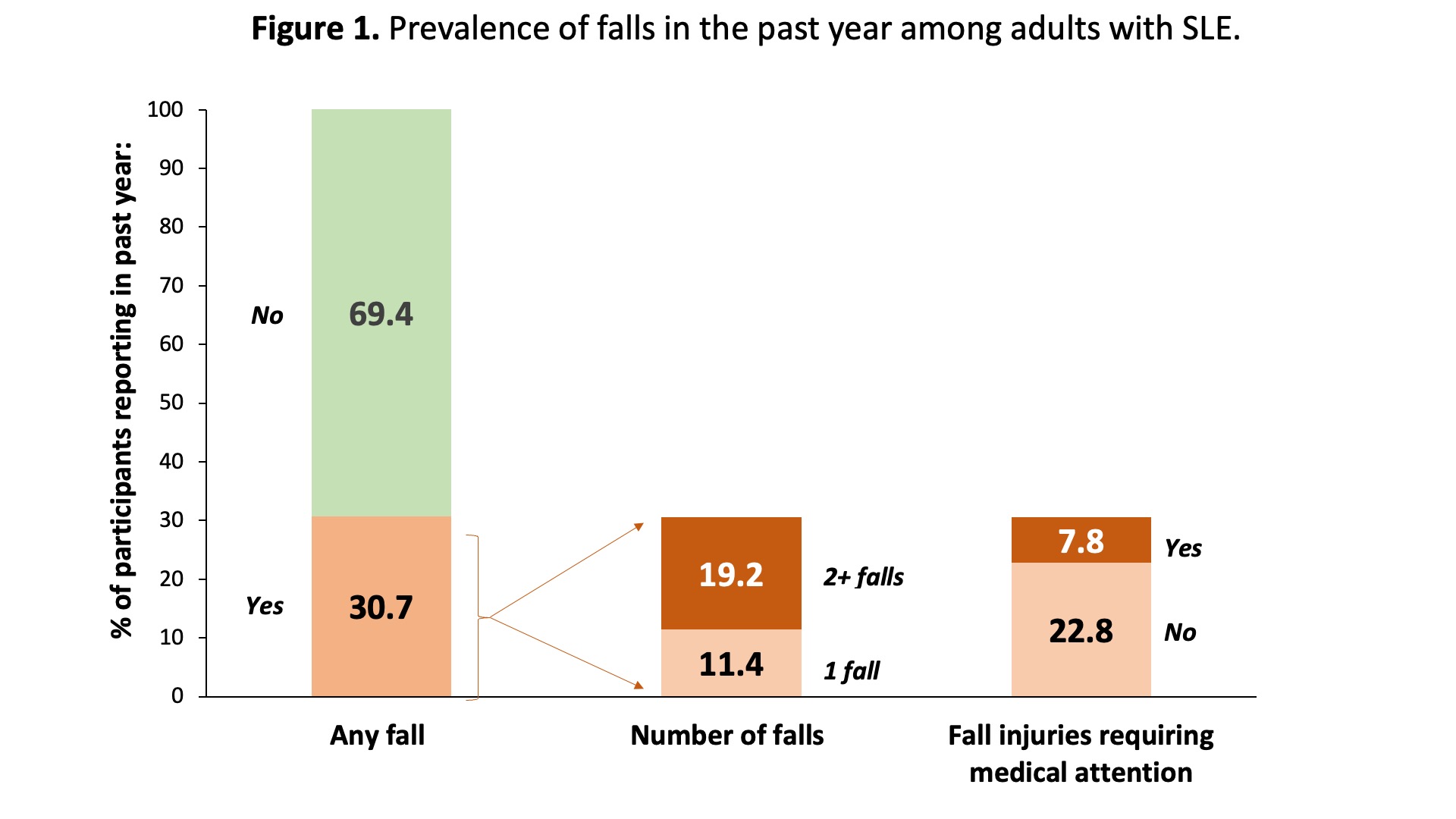
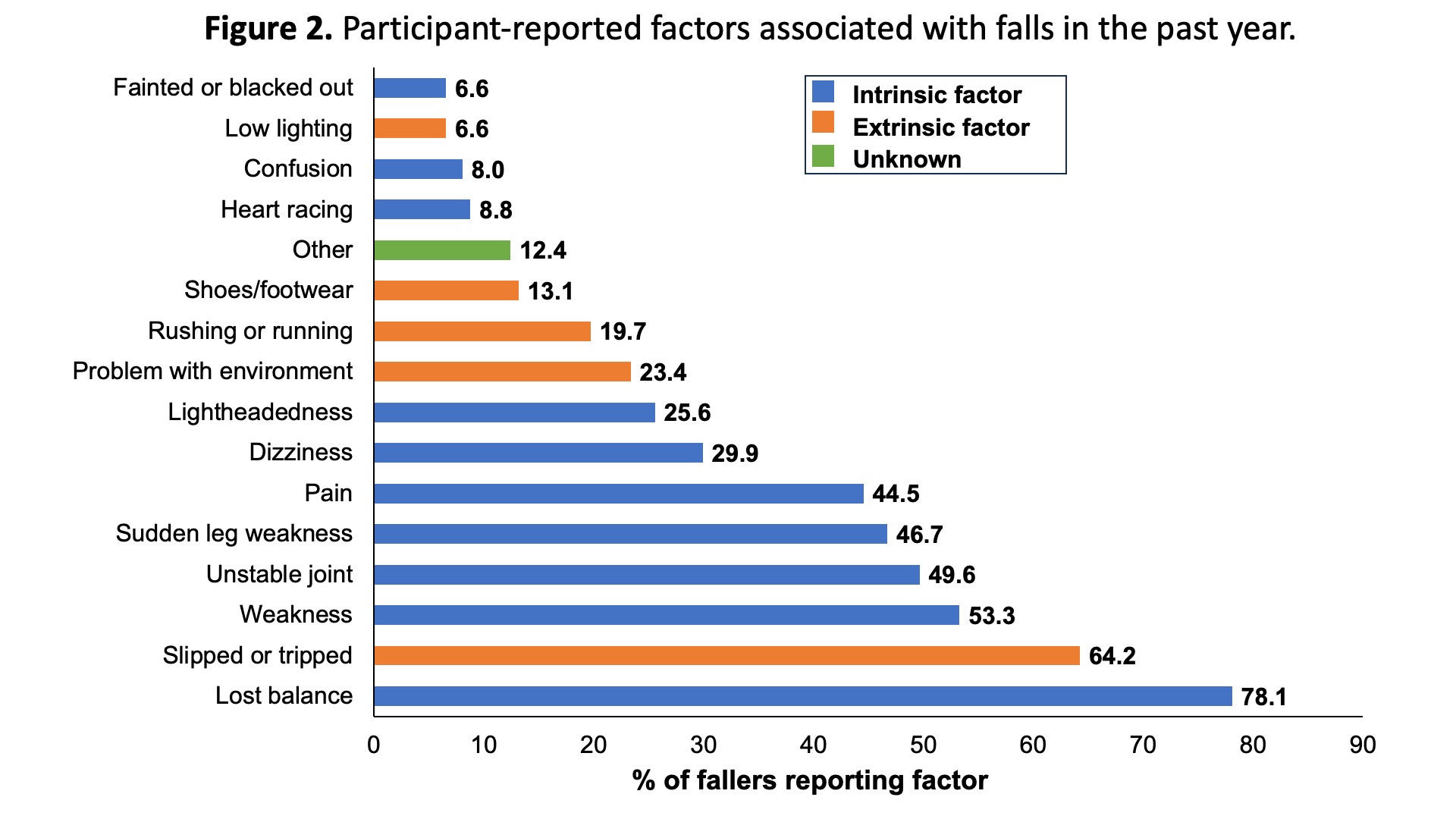
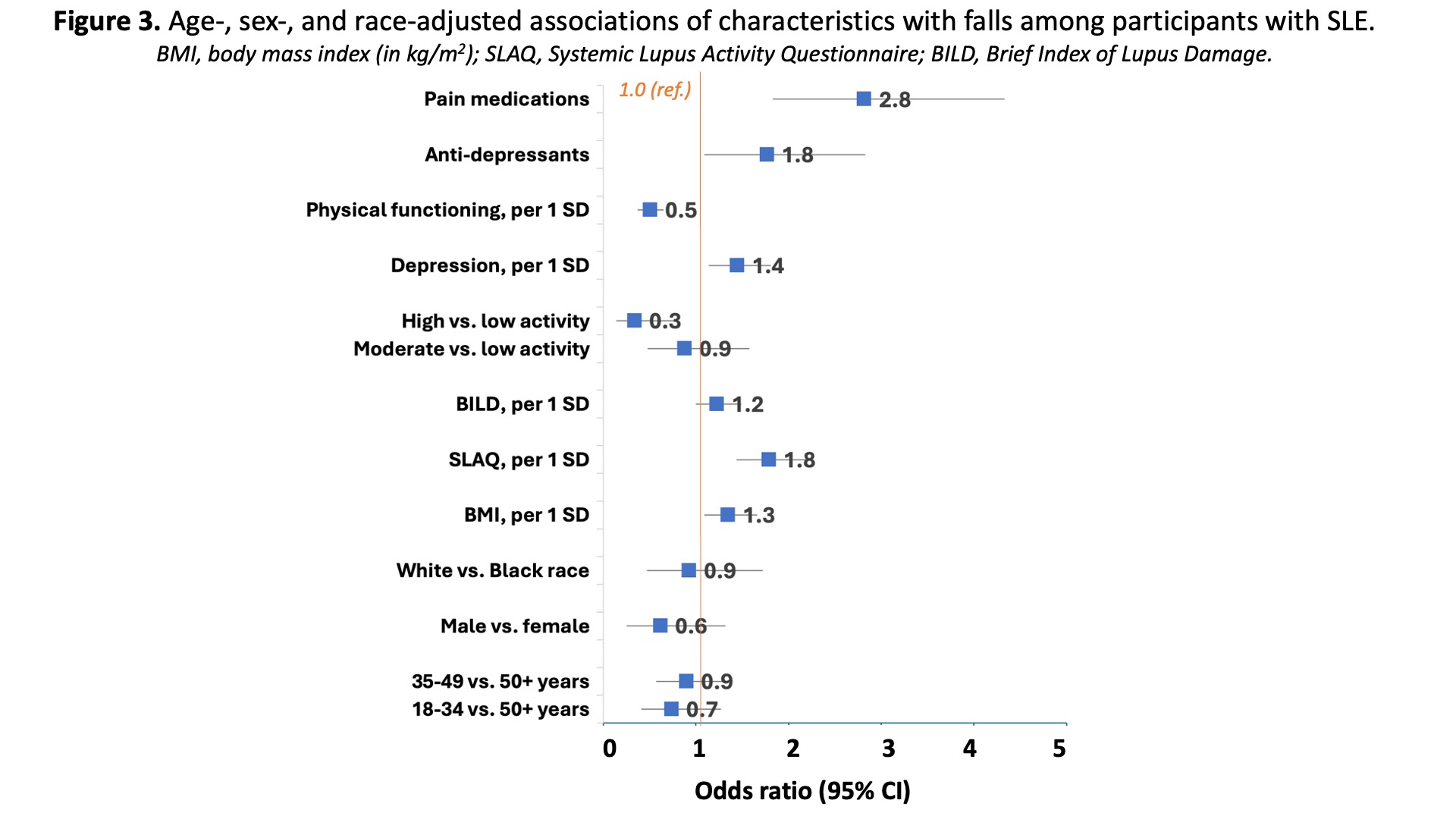
Results: Nearly one-third (30.7%) of participants (N=447; mean age, 46.2 years; 59.1% < 50 years old, 92% female, and 82% Black) reported at least one fall in the prior year. Among those who reported falling, the median number of falls (25th-75th percentile) was 2 (1-3) and 62.8% reported ³2 falls in the prior year; 25.6% of those who reported falling also reported requiring medical attention for the fall(s) (Figure 1). Fall-related factors that were intrinsic, including loss of balance, generalized weakness, unstable joints, leg weakness, and pain, were more commonly reported than factors that were extrinsic (Figure 2). After adjustment, higher disease activity and damage, higher BMI, greater depressive symptoms, and use of medications for depression and pain [particularly, opioid medications: aOR=4.46 (95% CI, 2.38, 8.56)] were all associated with higher odds of falls; higher self-rated physical functioning and higher physical activity were associated with lower odds of falls (Figure 3). Age, sex, race, and use of anti-hypertensives and benzodiazepines were not statistically significantly associated with odds of falls.
Conclusion: Regardless of age, falls may be common among adults with SLE, and our estimated annual risk of falls exceeds many published estimates from the U.S. older (³65 years) population. These falls may be due to modifiable intrinsic factors also present in older adults. Further, adults with SLE who have more active disease, more pain, lower physical activity, and greater depressive symptoms may be most at risk for falls. While more research is warranted, particularly exploring the consequences of falls among those with SLE, falls assessment and targeted interventions (such as physical therapy, mental health services, and pain control) among those with SLE may help prevent recurrent falls and their sequelae, including fractures, traumatic brain injury, and even death.
To cite this abstract in AMA style:
Plantinga L, Dunlop-Thomas C, Hoge C, Yazdany J, Bowling C. Epidemiology of Falls in a Diverse Cohort of Adults with SLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/epidemiology-of-falls-in-a-diverse-cohort-of-adults-with-sle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-of-falls-in-a-diverse-cohort-of-adults-with-sle/