Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Serum elevations of ACPA in the absence of inflammatory arthritis is a well-established risk factor for the future development of clinical RA. The lung is a mucosal site that has been implicated in the development of ACPA and RA. Our group has previously demonstrated that a significant proportion of serum ACPA+ individuals have high levels of lung inflammation prior to the development of clinical RA, as measured by lung imaging and elevations of inflammatory cytokines, complement fragments and ACPA in induced sputum. Herein, we aimed to identify immune cell subsets in the lung associated with serum ACPA+ individuals.
Methods: We included 15 serum ACPA+ At-Risk individuals and 10 healthy serum ACPA− controls. All study participants were not current smokers and did not have a clinical diagnosis of chronic lung disease. Serum ACPA positivity was determined based on an anti-CCP3 (IgG ELISA, Werfen) level greater than 3 standard deviations above the mean in a separate group of 120 controls without RA. We collected induced sputum using hypertonic saline and obtained the cell-rich fraction by dissociation with dithiothreitol and filtration with cell strainers. Fresh sputum cells were stained with fluorophore-conjugated antibodies, fixed with paraformaldehyde, and analyzed by an Aurora 5-laser spectral flow cytometer (Cytek Biosciences).
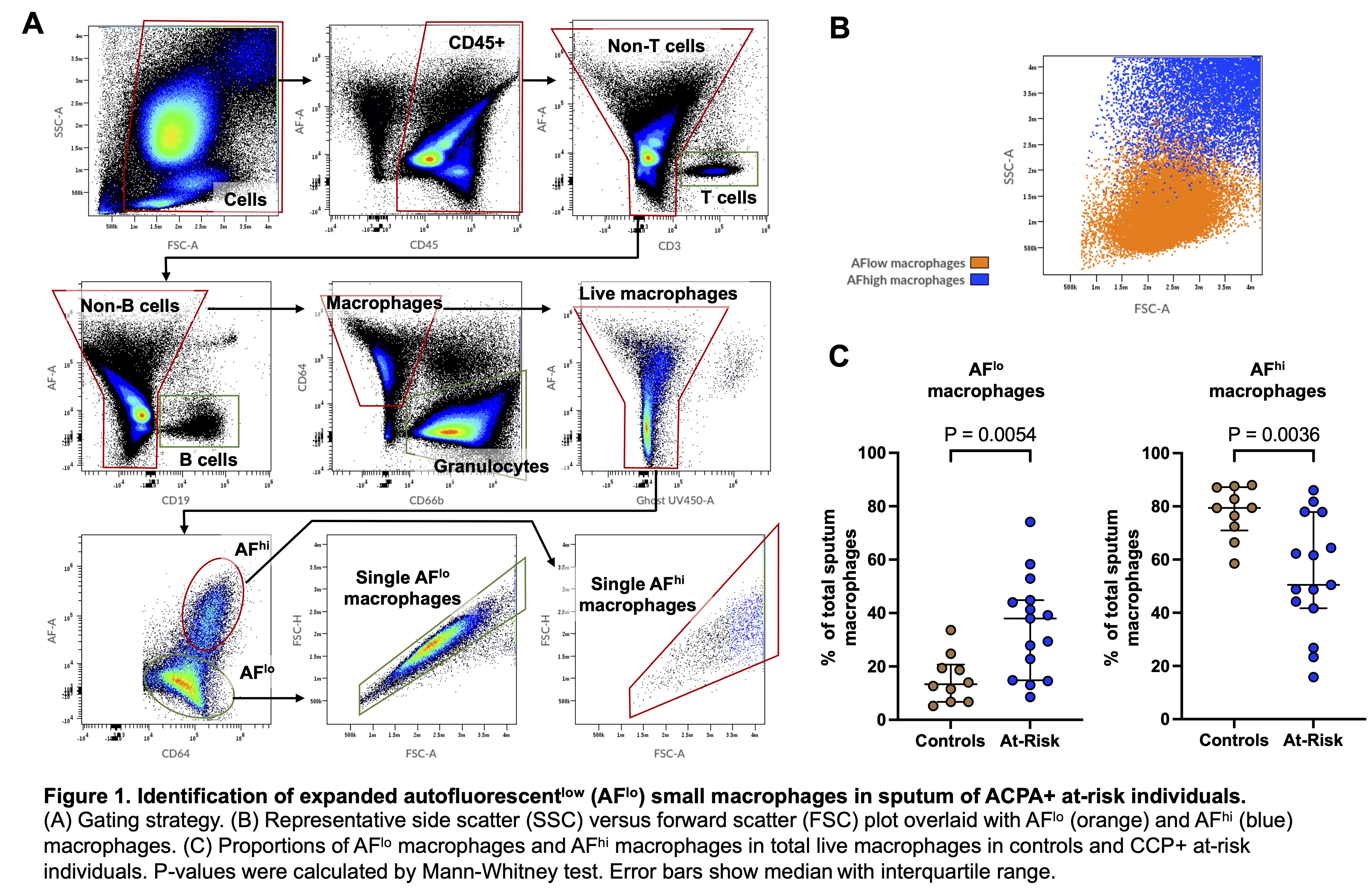
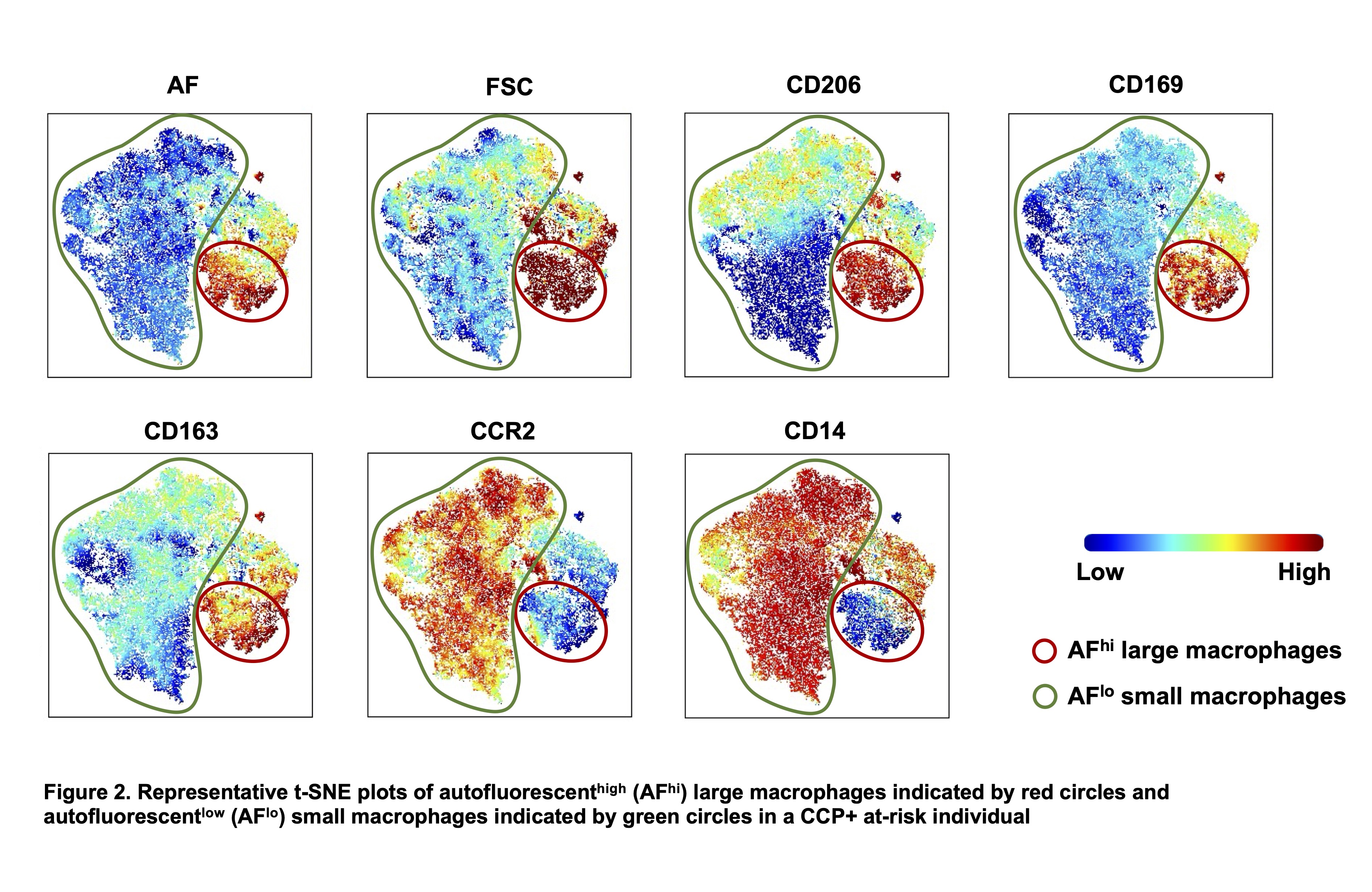
Results: There were no differences in sputum total cell count, % viability, or the proportions of neutrophils, dendritic cells, T cells, B cells and total macrophages between ACPA+ At-Risk individuals and controls. Notably, in macrophages (defined as CD45+CD66b−CD3−CD19−CD64+ cells) there were 2 distinct types of cells based on their autofluorescence intensities in both study groups (Figure 1A). Autofluorescent-low (AFlo) macrophages were smaller (forward scatter [FSC]lo) and less granular (side scatter [SSC]lo) compared to autofluorescent-high (AFhi) macrophages, which were larger (FSChi) and more granular (SSChi) (Figure 1B). Furthermore, the proportion of AFlo macrophages in sputum were significantly increased in serum ACPA+ At-Risk individuals compared to controls (p = 0.005) (Figure 1C), while the proportion of AFhi macrophages was decreased (p = 0.003). The t-SNE visualization of sputum macrophages revealed that AFhi macrophages expressed CD206, CD169, and CD163, suggesting ‘classical’ alveolar macrophages. In contrast, the AFlo macrophages highly expressed CCR2 and CD14 with no or low expressions of alveolar macrophage markers, suggesting these macrophages were monocyte-derived cells recently recruited from the blood to the lung (Figure 2).
Conclusion: Flow cytometry revealed that AFlo small macrophages, likely representing peripherally derived monocytes in the lung, were relatively expanded in the sputum in serum ACPA+ At-Risk individuals. This macrophage subset may play a key role in airway inflammation that in prior studies has been associated with serum ACPA+ At-Risk individuals. Further studies are needed to investigate the functional properties of this macrophage subset in the lung, including its relationship to local (i.e. lung) generation of autoantibodies and inflammation, and to explore its association with RA progression.
To cite this abstract in AMA style:
Takada H, Hattel B, Feser M, Moss L, Okamoto Y, Gillespie M, Savage A, Torgerson T, Holers V, Deane K, Demoruelle K. Flow Cytometry of Cells Within Induced Sputum from Individuals At-Risk for RA Reveals Relative Expansion of Small Macrophages [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/flow-cytometry-of-cells-within-induced-sputum-from-individuals-at-risk-for-ra-reveals-relative-expansion-of-small-macrophages/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/flow-cytometry-of-cells-within-induced-sputum-from-individuals-at-risk-for-ra-reveals-relative-expansion-of-small-macrophages/