Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Subdoligranulum didolesgii, S. dido 7, is present in a subset of individuals who are at-risk for RA (termed ‘ARI’) and who have clinical RA, activates CD4+ T cells in humans with RA, and is bound by dual family IgA/IgG monoclonal antibodies derived from ARI. S. dido 7 translocates across the intestinal barrier and leads to inflammatory arthritis (IA) and RA-relevant antibodies in mono-colonized germ-free mice. Intestinal permeability and increased abundance of other bacteria such as Prevotella copri are also observed in ARI and RA. To link these observations to prospective development of RA, we hypothesized that intestinal barrier permeability, fecal S. dido 7, and additional dysbiosis will associate with transition from AR to RA.
Methods: Stool and sera were prospectively collected from 3 groups: 1) ARI, defined as serum CCP+ with no past nor current IA at baseline (n=64), 2) Early RA, defined as untreated individuals with CCP+ RA (2010 ACR/EULAR criteria) within 12 months of diagnosis (n=6), and 3) Controls, defined as healthy individuals without IA or RF/CCP (n=49). Longitudinal samples were collected from ARI over 5 years and sub-grouped as those who convert to IA/RA (converters) and those who did not (non-converters). Fecal S. dido 7 and serum CCP3, zonulin and sCD14 were measured by quantitative PCR and ELISA, respectively. Shotgun metagenomic sequencing of stool was performed via Illumina and processed via MetaPhlAn and HuMAnN.
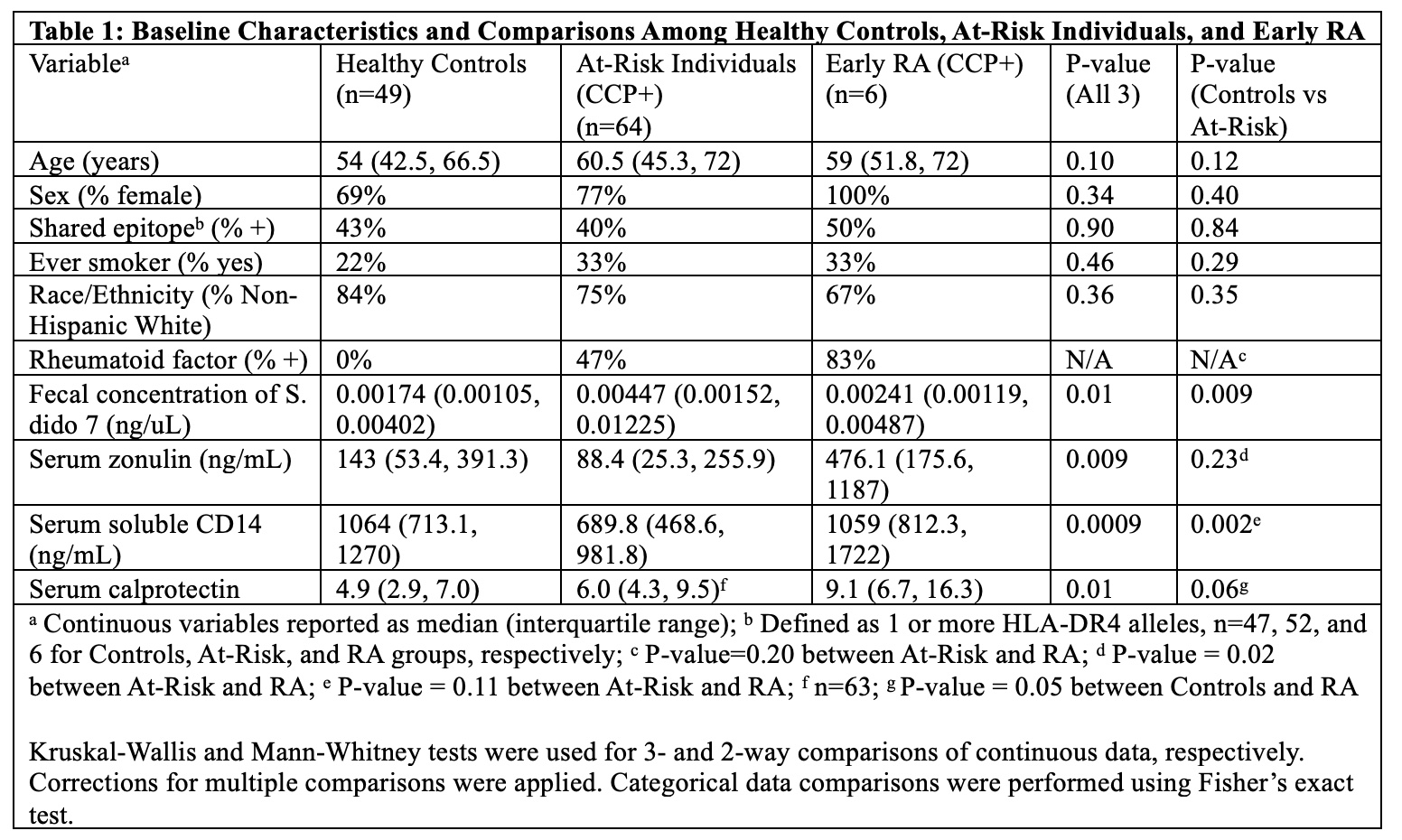
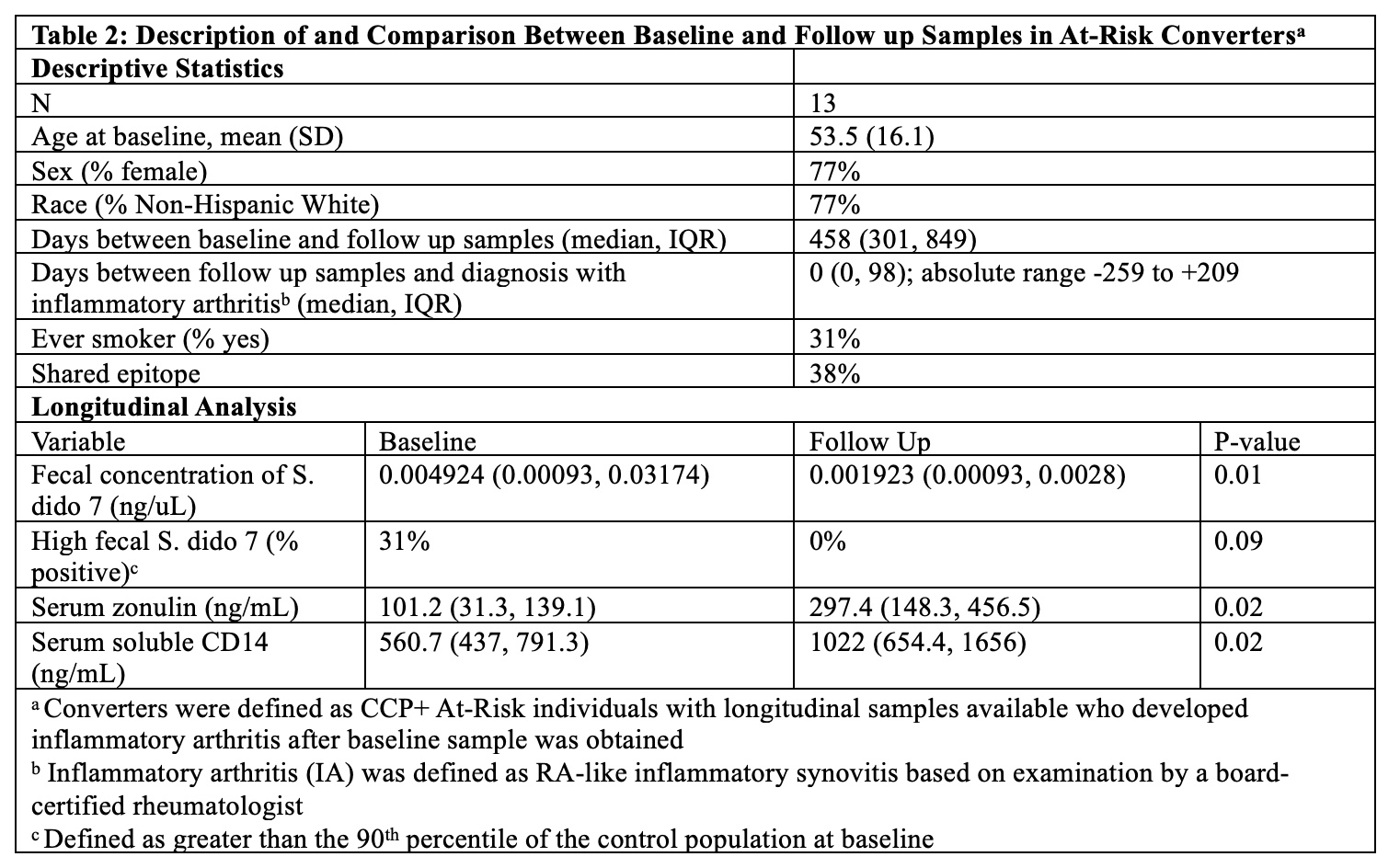
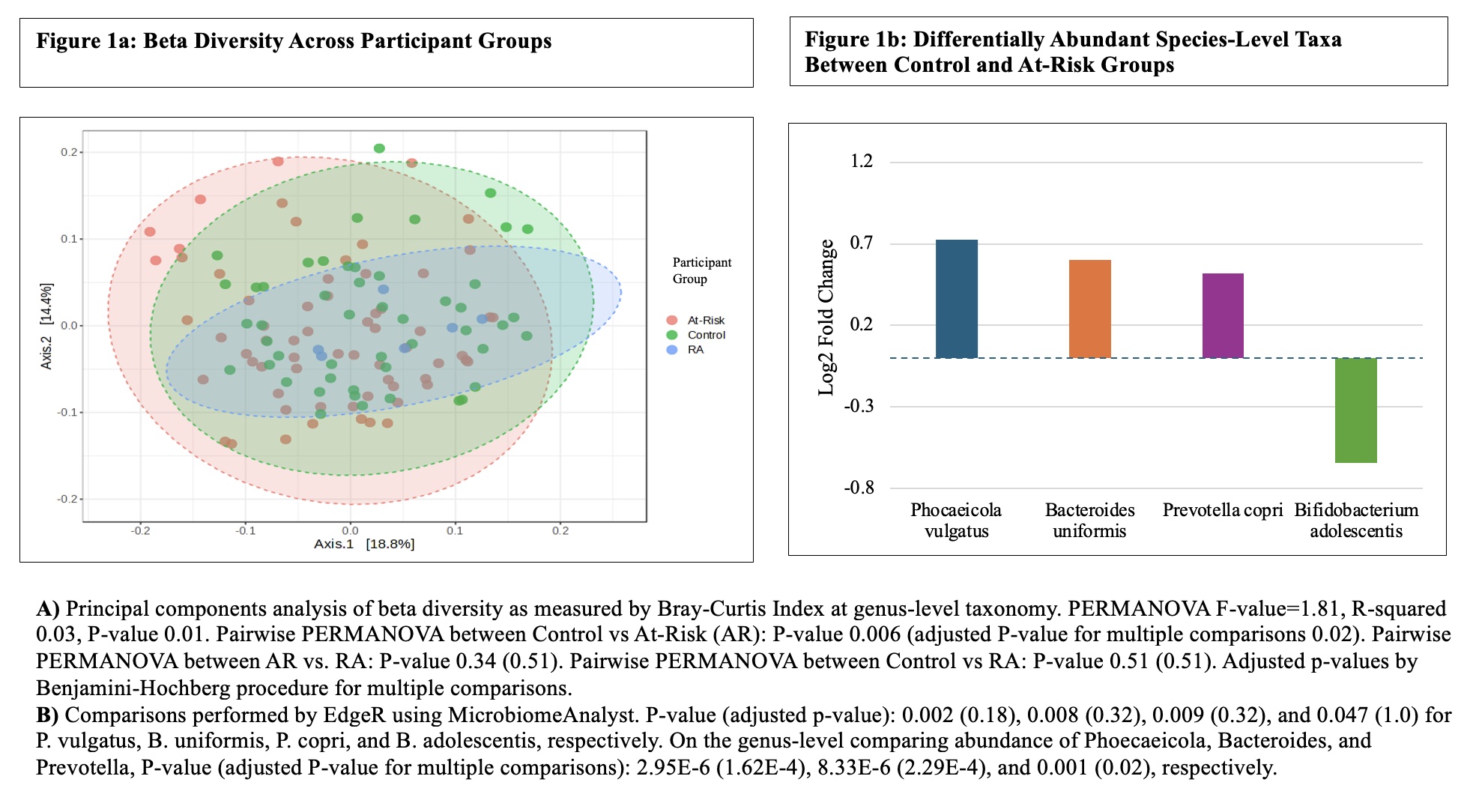
Results: Baseline fecal concentration of S. dido 7 was 2.6-fold higher in ARI and 1.4-fold higher in early RA compared to controls, P=0.01, Table 1. Serum zonulin and sCD14 were lower in ARI compared to controls and RA, P< 0.01, Table 1. S. dido 7 negatively associated with zonulin and sCD14, Spearman r = -0.36 and -0.19, P < 0.01 and 0.04, respectively, and was positively associated with CCP3, r=0.2, P=0.03. Alpha diversity of the fecal microbiome did not differ across groups at baseline, but beta diversity was significantly different (Figure 1a); by pairwise comparison, there was no baseline difference between converters and non-converters. ARI exhibited a greater abundance of Prevotella, Phocaeicola, and Bacteroides genera and lower abundance of Bifidobacterium adolescentis compared to controls (Figure 1b). There was a trend for S. dido 7 levels with Dietzia cercidiphylli, r=0.31, P= 0.05. Longitudinally, at follow up closest to time of diagnosis with IA/RA (median 458 days from baseline), converters showed decreased fecal S. dido 7 and increased zonulin and sCD14 compared to baseline (Table 2).
Conclusion: Our data confirm that S. dido 7 is elevated in ARI. However, in converters, S. dido 7 concentration decreases over time (though not to the level of controls) in association with increased intestinal permeability. This is indicative of active immune regulation of this bacterium possibly leading to development of IA/RA. Although we confirm dysbiosis at baseline in ARI, including increased abundance of P. copri, ongoing analysis of longitudinal bacterial metagenomics data will determine additional bacterial abundance changes with conversion to IA/RA and potentially identify additional associations with intestinal permeability and S. dido 7.
To cite this abstract in AMA style:
Cole L, Liu S, Allen B, Feser M, Demoruelle K, Deane K, Holers M, Kuhn K. Arthritogenic Subdoligranulum (S. Dido 7) Is Increased in Individuals At-Risk for and with Early RA and Decreases over Time During Development of Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/arthritogenic-subdoligranulum-s-dido-7-is-increased-in-individuals-at-risk-for-and-with-early-ra-and-decreases-over-time-during-development-of-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/arthritogenic-subdoligranulum-s-dido-7-is-increased-in-individuals-at-risk-for-and-with-early-ra-and-decreases-over-time-during-development-of-inflammatory-arthritis/