Session Information
Date: Tuesday, November 14, 2023
Title: (2352–2369) Systemic Sclerosis & Related Disorders – Clinical Poster III: Translational Science
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: In patients with systemic sclerosis (SSc), progression of interstitial lung disease (ILD) is associated with an increased mortality. Since the course of SSc-ILD is highly variable, it is critical to predict the progression of ILD in clinical practice as well as in clinical trial setting. Previously reported risk factors for ILD progression include male, progression of skin thickness in diffuse cutaneous SSc (dcSSc), short SSc duration, anti-Scl-70, and elevated inflammatory markers and Krebs von den Lungen-6 (KL-6). The aim of this study was to examine performance of inflammatory markers and KL-6 to efficiently enrich patients who subsequently experience ILD progression in SSc patients using a single-center prospective cohort.
Methods: Two cohorts, including patients with dcSSc (n=109) and those with SSc-ILD (n=136), were selected from our prospective SSc registry. 87 patients with dcSSc and ILD were included in both cohorts. C-reactive protein (CRP) ≥6 mg/L and erythrocyte sedimentation rate (ESR) ≥28 mm/hour were used as increased inflammatory markers, and a cutoff point of increased KL-6 was provisionally set at 1,000 U/mL. ILD progression was defined as the first event developing progressive fibrosing ILD (PF-ILD) or progressive pulmonary fibrosis (PPF). Receiver Operating Characteristic Curve (ROC) analysis was conducted to determine the sensitivity, specificity and area under the curves (AUCs) and the Youden index was used to identify the appropriate cutoff. Cumulative rates free from ILD progression were assessed using Kaplan-Meier analysis and statistical comparisons were made using log-rank test.
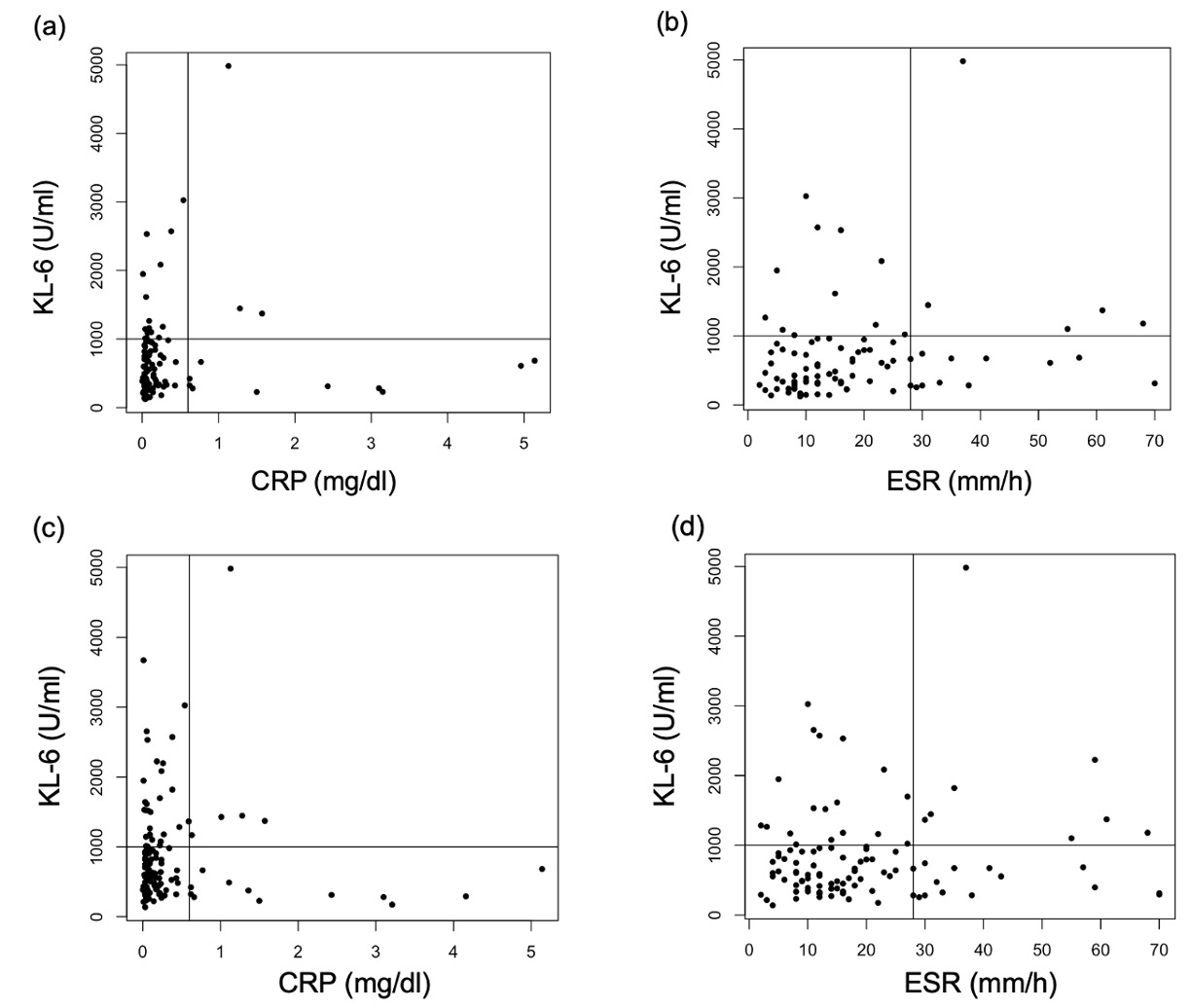
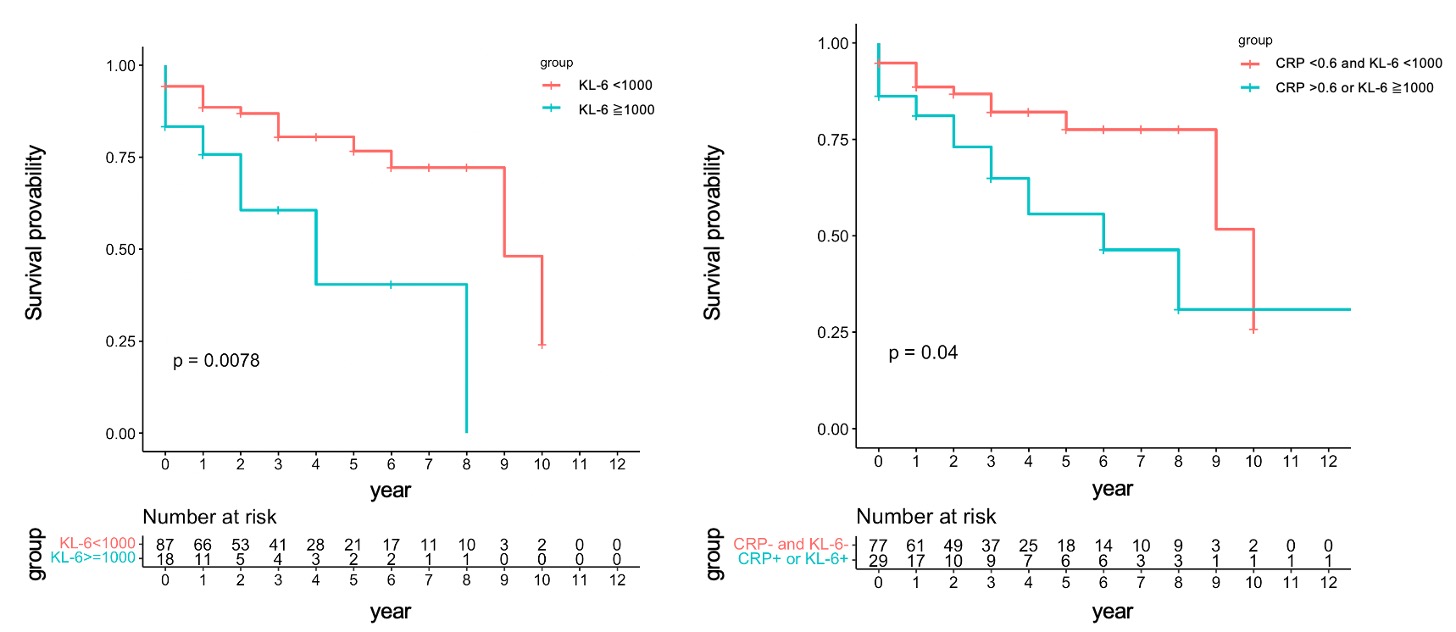
Results: Median disease duration at baseline was 15.0 and 23.5 months in dcSSc and SSc-ILD cohorts, respectively. In dcSSc cohort, 27 (25%) and 22 (20%) patients developed PF-ILD and PPF during median follow-up of 37 month, respectively; and 43 (31%) and 36 (26%) in SSc-ILD cohort developed PF-ILD and PPF during median follow-up of 43.5 months, respectively. There was no correlation between inflammatory markers and KL-6 (Figure 1). The specificity of CRP, ESR and KL-6 to predict ILD progression was favorable (74-88%), but sensitivity of CRP and ESR was low (9-15%). KL-6 provided better sensitivity (24-45%) (Table 1). The combination of CRP and KL-6 showed the best AUCs (0.54-0.62), with increased sensitivity (33-52%) while mainlining acceptable specificity (69-76%). Regardless of how ILD progression is defined, Kaplan-Meier analysis showed that the patients with increased KL-6 experienced ILD progression more frequently than those without. The same trend was observed for the KL-6/CRP combination (Figure 2). Optimal cut-offs of KL-6 to predict PF-ILD and PPF were found to be lower than provisional cut-off in dcSSc (~610 U/mL) and SSc-ILD (820 U/mL) and the models using these data-driven cut-offs improved AUCs compared to provisional setting.
Conclusion: We propose use of combination of KL-6 and CRP in the inclusion criteria for enriching “at risk” patients in clinical trials for SSc, while optimal cut-off need to be further defined using different multicenter cohorts.
To cite this abstract in AMA style:
Yomono K, Khanna D, Kuwana M. Optimal Combination of Circulating Biomarkers for Predicting the Progression of Interstitial Lung Disease in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/optimal-combination-of-circulating-biomarkers-for-predicting-the-progression-of-interstitial-lung-disease-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/optimal-combination-of-circulating-biomarkers-for-predicting-the-progression-of-interstitial-lung-disease-in-patients-with-systemic-sclerosis/