Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
b>
Background/Purpose: Patients with pure membranous lupus nephritis (LN) are known to have a different disease course than those with proliferative disease. The aim of this study is to determine the differences in short and long term outcomes between patients with pure membranous LN and those with proliferative LN, in terms of achieving complete proteinuria recovery (CPR), time to CPR and a composite of poor renal outcome.
Methods: This is a retrospective analysis of patients followed prospectively at a single large Lupus cohort who had biopsy-proven Class V, Class IV+V or III+V or isolated class III or IV LN. We included only first patient-biopsy. The baseline visit corresponds to the visit with highest level of proteinuria in relation with the kidney biopsy visit. Baseline characteristics of patients (demographic data, laboratory results, clinical features and treatment protocols) were analyzed. The primary endpoint, CPR, was defined as proteinuria < 500 mg/24 h. CPR was evaluated at 1 year and 2 years for the different LN classes. The time to CPR was assessed with a Kaplan-Meier curve. Time to a composite of poor renal outcome (eGFR ≤ 15 mL/min/1.73m2, chronic dialysis or kidney transplant) was also evaluated. These outcomes were compared between patients with pure membranous LN and those with proliferative disease (including mixed biopsies; class III+V or IV+V).
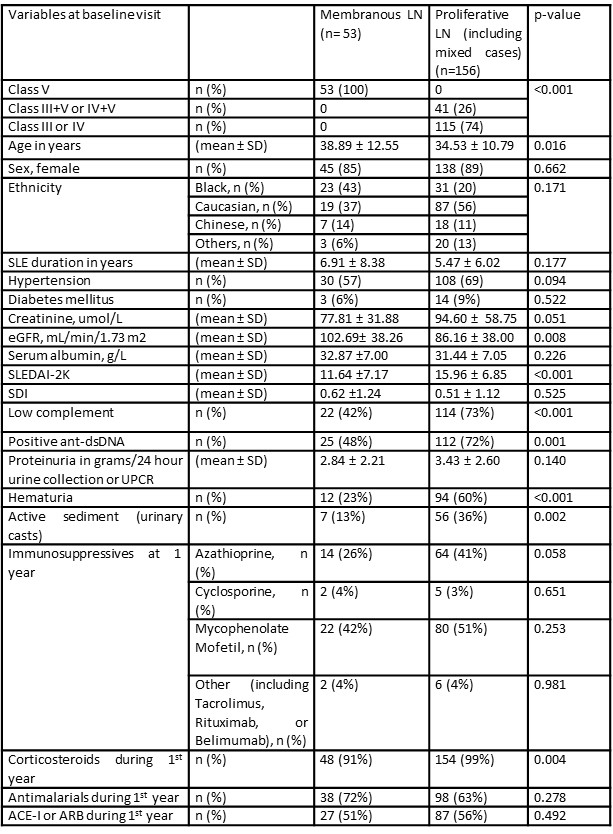
Results: 209 patients fulfilled the above criteria with at least 2 years of follow up after the baseline visit. Of these, 53 had pure membranous LN, 41 had mixed disease (class IV+V or III+V), and 115 had pure proliferative disease (class III or IV). Overall, 156 patients had proliferative disease on biopsy. Patients with pure membranous LN were slightly older at baseline than those with proliferative disease (38.89 Vs 34.53 years, p= 0.016). They also had a higher eGFR (102.69 Vs 86.16 mL/min/1.73 m2, p= 0.008) and a lower SLEDAI-2K score (11.64 Vs 15.96, p < 0.001) at baseline. Proliferative LN patients tended to be more serologically active (p= 0.001 for anti-dsDNA and < 0.001 for low complements) and had more hematuria (p< 0.001) and urinary casts (p=0.002). There were no significant differences in the baseline proteinuria levels between the two groups. Mycophenolate was the most commonly used drug in the standard of care therapy. Less patients with pure membranous LN received corticosteroids during the first year after the baseline visit (p= 0.004) (Table 1).
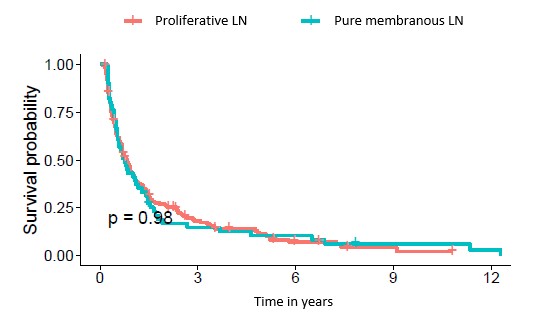
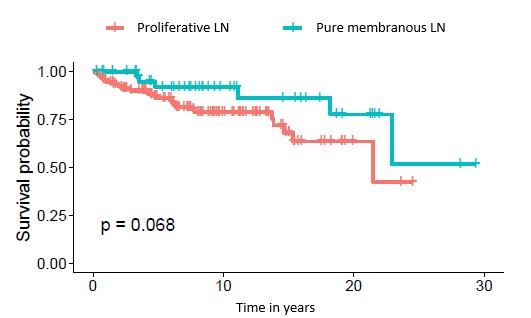
There were no differences in the CPR at 1 year (51% for both groups) or at 2 years (66% for membranous and 62% for proliferative disease, p= 0.660) between the 2 groups. Time to CPR was also comparable (Figure 1). Time to the composite of poor renal outcome showed a trend in favor of pure membranous patients, but did not meet statistical significance (Figure 2).
Conclusion: CPR at one and two years, and time to CPR were similar in patients with pure membranous LN and those with proliferative disease. Time to a composite of poor renal outcome was not significantly different between the two groups. These results show that pure membranous lupus nephritis may be associated with ominous long term outcomes.
To cite this abstract in AMA style:
Kharouf F, Diaz Martinez J, Gladman D, Touma Z. Short and Long Term Outcomes of Patients with Pure Membranous Lupus Nephritis Compared to Patients with Proliferative Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/short-and-long-term-outcomes-of-patients-with-pure-membranous-lupus-nephritis-compared-to-patients-with-proliferative-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/short-and-long-term-outcomes-of-patients-with-pure-membranous-lupus-nephritis-compared-to-patients-with-proliferative-disease/