Session Information
Date: Tuesday, November 14, 2023
Title: (2039–2060) Pediatric Rheumatology – Clinical Poster III: Potpourri
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Juvenile recurrent parotitis (JRP) is characterized by non-obstructive, non-suppurative inflammation of the parotid glands of unknown etiology. The onset of symptoms occurs typically between ages 3-6 and there is a tendency for spontaneous resolution after puberty. Patients are primarily managed by Otolaryngology and approximately 2/3 of patients respond to sialadenoscopy after failing conservative measures, however additional medical therapies are sometimes required. The purpose of this study was to analyze the subset of patients who are referred to rheumatology and to describe the immunosuppressive treatment utilized.
Methods: With approval from our Institutional Review Board, patients were identified via our electronic medical records (EMR) using the ICD-9 and ICD-10 codes for “recurrent parotitis” and “parotitis” between 2013 and 2023 who were seen by rheumatology. Patients 21 years and younger, with at least 3 episodes of parotitis per year or 2 within 6 months, were included. Demographic and clinical information was obtained. Treatment response was determined as complete remission (no episodes in 12 months) or partial response (less than 3 episodes per year or less than 2 episodes per 6 months). Data were evaluated using standard descriptive statistics.
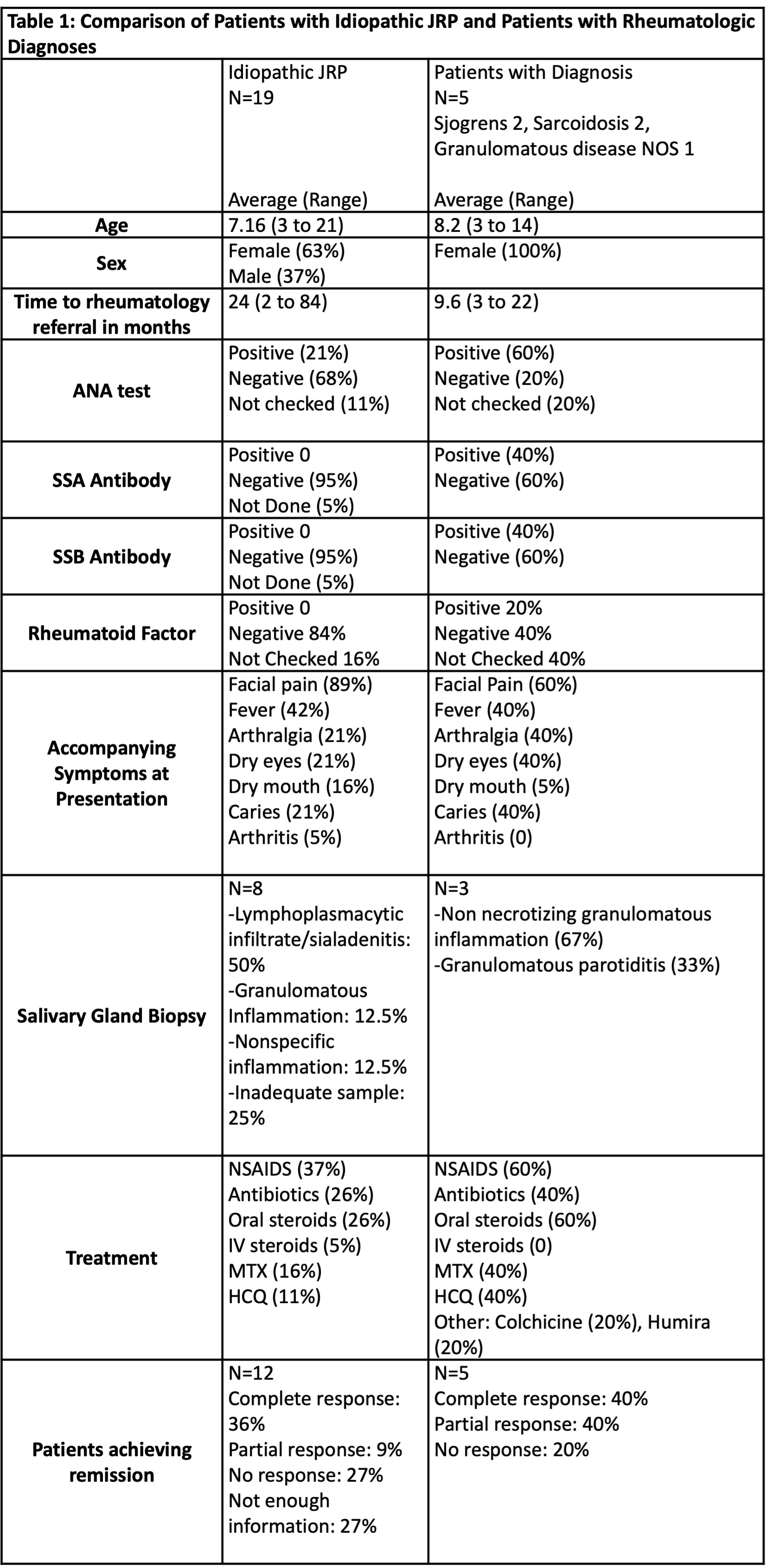
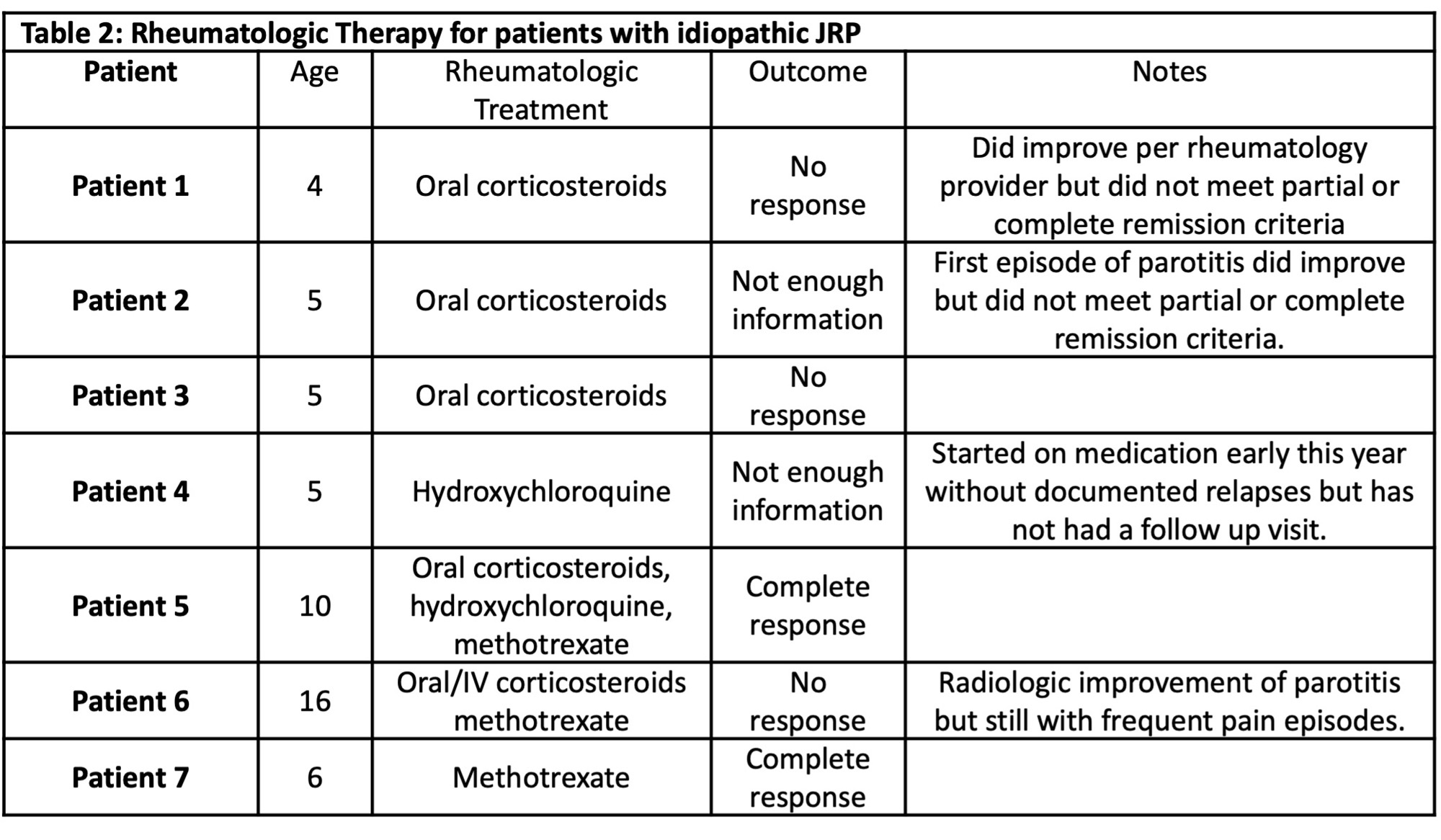
Results: A total of 26 patients met inclusion criteria. Average age was 7 (range 3-21), majority were female (73%), white (77%), and non-Hispanic (62%). Average total episodes of parotitis were 7 (range 2-42), with 4 episodes per year on average. Bilateral parotitis was noted in 81%. Average duration of symptoms prior to referral to rheumatology was 20 months (range 2-84). The more common referral reasons included recurrence (35%) and concern for autoimmune etiology based on laboratory evaluation or biopsy (27%). Five (18.6%) patients had a rheumatologic diagnosis: 2 with Sjogren’s syndrome, 2 with sarcoidosis and 1 with unspecified granulomatous parotitis. Among patients referred, ANA was checked in 23 of 26 patients of which 57% were positive. Fifty percent of patients in the group underwent biopsy. Ten out of 26 patients underwent sialadenoscopy with steroid injection, 6 with Kenalog (60%), 3 with ciprofloxacin/dexamethasone (30%), and one with both (10%). Patients were followed for a mean of 25.7 months (range 0.5 -97).Of those without rheumatologic or infectious diagnosis, 7 (37%) patients received immunomodulatory treatment of which 2 achieved complete remission (29%). Treatment included corticosteroids, NSAID, methotrexate, and hydroxychloroquine (Table 2). Among the 12 patients without therapy, 2 (17%) had complete remission.
Conclusion: Patients with JRP were referred to rheumatology clinic due to suspicion for autoimmune conditions or refractory course. In this cohort only a small number of patients had a rheumatologic diagnosis and few idiopathic JRP received immunomodulatory therapy. A subset of children with recurrent parotitis may benefit from rheumatologic consultation and possible treatment with anti-inflammatory and immunomodulatory therapy. Limitation of this study include its retrospective nature, small number of patients and short follow up periods.
To cite this abstract in AMA style:
Pina Y, Lambert E, Pereira M, De Guzman M. An Analysis of Recurrent Parotitis Patients Referred to Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/an-analysis-of-recurrent-parotitis-patients-referred-to-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-analysis-of-recurrent-parotitis-patients-referred-to-rheumatology-clinic/