Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Previous studies have suggested low-level chronic inflammation plays a key role in knee osteoarthritis (OA) development and progression. In the present study, we set out to investigate, via mass cytometry, differences in circulating blood immunophenotypes in moderate-stage OA patients compared to controls, and to investigate differences in baseline immunophenotypes in OA patients who later experienced radiographic or pain progression within the subsequent 2 years.
Methods: Early OA patient samples were obtained from the Oklahoma SOONER OA cohort, defined as baseline K/L grade 0-3 and knee pain on most days for the past 6 months. Fixed-flexion radiographs and WOMAC information from visits every 6 months was analyzed. Radiographic progressors were defined as having mean medial TF joint space narrowing of ≥0.7mm within 24 months. Pain progressors were defined as having a WOMAC pain subscale worsening of at least 10 points on a 0-100 normalized scale within 24 months. Matched controls were obtained from the Oklahoma Immune Cohort. The final analysis included 13 OA patients and 13 controls. Among OA patients, 4/13 were radiographic progressors and 5/13 were pain progressors. Baseline blood samples were stained with Maxpar Direct immune profiling assay kit (Fluidigm), then subjected to mass cytometry analysis. Quantitative analysis of 37 immune cell populations was then performed and group differences defined with a student T-test. Generalized logistic models were then developed to classify patients into the above groups.
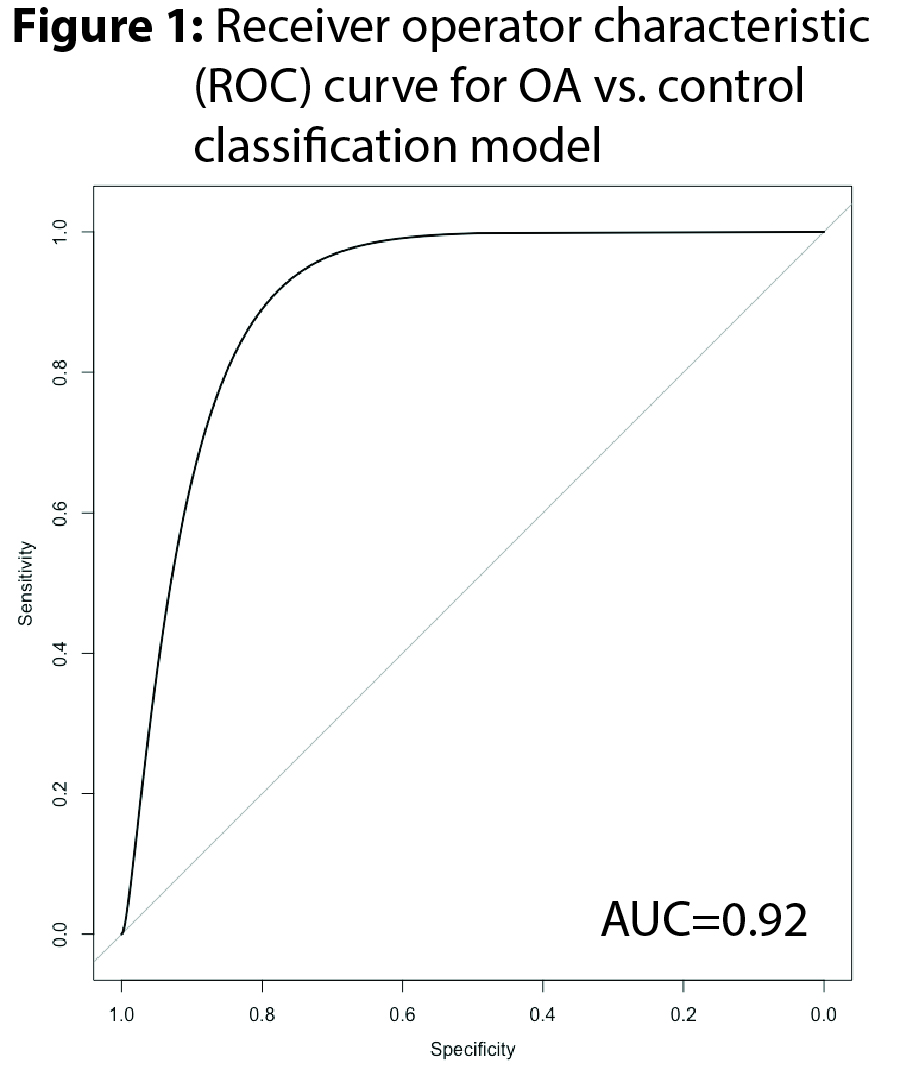
Results: Comparing all OA patients to controls, there were increases in MAIT/NK T cells (OA: 3.3±0.6 vs. healthy: 1.5±0.2, mean % of parent cell population±SEM, P=0.02) (Table 1) and eosinophils (4.2±0.7 vs. 1.6±0.5, P=0.01), as well as decreases in classical- (91.6±0.7 vs. 94.3±0.7, P=0.03) and transitional-monocytes (6.8±0.5 vs. 4.8±0.6, P=0.03) noted. Radiographic progressors were characterized by baseline decreases plasmacytoid- (35.8±2.5 vs. 32.6±3.2, P=0.03) and increases in myeloid-dendritic cells (64.2±2.5 vs. 67.5±3.2, P=0.03). Pain progressors were found to have increases in Th17 T-cells (13.0±2 vs. 7.4±0.6, P=0.02). A machine learning logistic model was then trained to differentiate OA patients from healthy controls and underwent 3-fold cross-validation with internal tuning. The model demonstrated 84% accuracy with a receiver operator characteristic area under the curve (ROC-AUC) of 0.92 (Figure 1).
Conclusion: Our study is the first to perform deep immunophenotyping of peripheral blood on a small group of OA patients and well-matched controls. The results suggest that significant alterations in certain immune cell subpopulations are present among OA patients and at baseline prior to future radiographic or pain progression, and provide additional support for the hypothesis that OA represents a systemic disease characterized by low-level immune dysregulation. Future research should confirm our findings and investigate the pathophysiological consequences of these variations.
To cite this abstract in AMA style:
Dyson G, Barrett M, Jeffries M. Deep Immunophenotyping of Osteoarthritis Patients Demonstrates Baseline Alterations in Monocyte Populations in OA, Dendritic Cell Subpopulations Among Radiographic Progressors, and Th17 Cells Among Pain Progressors [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/deep-immunophenotyping-of-osteoarthritis-patients-demonstrates-baseline-alterations-in-monocyte-populations-in-oa-dendritic-cell-subpopulations-among-radiographic-progressors-and-th17-cells-among-pa/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/deep-immunophenotyping-of-osteoarthritis-patients-demonstrates-baseline-alterations-in-monocyte-populations-in-oa-dendritic-cell-subpopulations-among-radiographic-progressors-and-th17-cells-among-pa/