Session Information
Date: Tuesday, November 14, 2023
Title: (1913–1944) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Sarcoidosis is a systemic granulomatous inflammatory disease that can involve multiple organ systems. Rarely, sarcoidosis can involve the upper respiratory tract including the sinonasal region. Symptoms easily mimic those of allergic or atrophic rhinitis, bacterial sinusitis; therefore, commonly leading to misdiagnosis. Here, we aim to identify comorbidities in this subset of sarcoidosis patients to raise a higher clinical suspicion for this diagnosis in a higher risk population; thereby, avoiding a delay in appropriate management.
Methods: The National Inpatient Sample (NIS) from 2003 to 2014 was queried to identify patients diagnosed with sarcoidosis (ICD-9: 135). Patients with sarcoidosis were categorized into two groups based on whether they had comorbid sinonasal diagnoses (including acute or chronic sinusitis, nasal polyps, deviated nasal septum, epistaxis, or nasal mucositis). Univariate and multivariate logistic analyses were conducted to compare patient and hospital characteristics as well as Elixhauser comorbidities between the two groups.
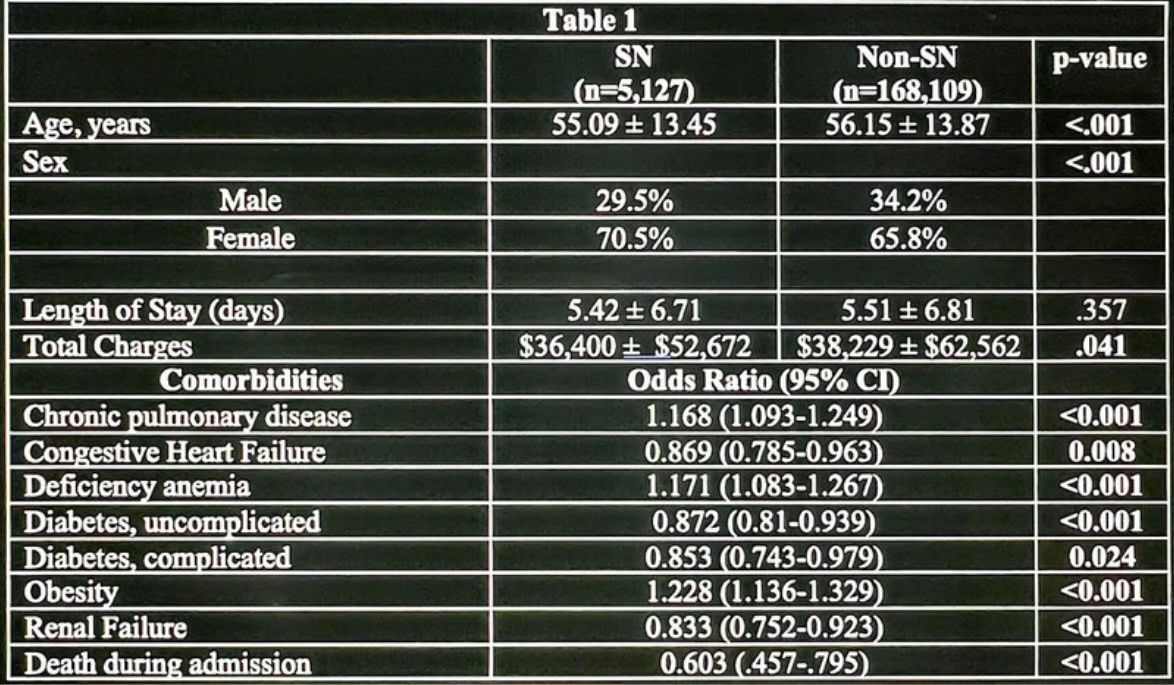
Results: A total of 173,236 sarcoidosis patients were included, 5,127 (3.0%) of whom had a comorbid SN diagnosis. Patients with SN involvement were younger (55.09 years ± 13.45 vs 56.15 ± 13.87, p< .001), more often female (70.5% vs 65.8%) than their non-SN counterparts. After accounting for demographics, patients who developed SN diagnoses were more likely to have chronic pulmonary disease (OR [95% CI]: 1.168 [1.093-1.249], p< 0.001), deficiency anemia (1.171 [1.083-1.267], p< 0.001), and be obese (1.228 [1.136-1.329], p< 0.001). However, those with congestive heart failure (0.869 [0.785-0.963], p=0.008), diabetes (0.872 [0.810-0.939], p< 0.001), or renal failure (0.833 [0.752-0.923], p< 0.001) were less likely to have a SN comorbidity. Patients with SN involvement had decreased hospital charges ($36,400 ± $52,672 vs $38,229 ± $62,562, p=0.041), but did not significantly differ on length of stay (5.42 ± 6.71 vs 5.51 ± 6.8, p=0.357) than those without a SN diagnosis. Patients with SN involvement of sarcoidosis were also less likely to die during their hospital admission than their non-SN counterparts (0.603[.457-.795], p< 0.001) (table 1).
Conclusion: Our findings suggest that the management of sarcoidosis patients with chronic pulmonary disease, deficiency anemia, or obesity should include a high index of suspicion for comorbid SN diagnoses. However, SN involvement does not increase sarcoid patients’ risk for death, prolonged stay, or increased hospital charges. Further research is warranted to investigate underlying mechanisms and clinical implications of SN involvement in sarcoidosis.
To cite this abstract in AMA style:
Kokush E, Salim M, Capitle E, Khianey R, Kalyoussef E. Sinonasal Sarcoidosis Associated with Chronic Pulmonary Disease, Deficiency Anemias, and Obesity [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sinonasal-sarcoidosis-associated-with-chronic-pulmonary-disease-deficiency-anemias-and-obesity/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sinonasal-sarcoidosis-associated-with-chronic-pulmonary-disease-deficiency-anemias-and-obesity/