Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: According to recent ACR and EULAR rheumatoid arthritis (RA) guidelines, glucocorticoids (GCs) should only be used for brief periods or not at all. Our aim was to investigate U.S. real-world GC usage patterns in elderly early RA patients, who are especially likely to suffer from adverse events, and assess the relationship between GC initiation, entrance into rheumatologic care, and subsequent, long-term GC use.
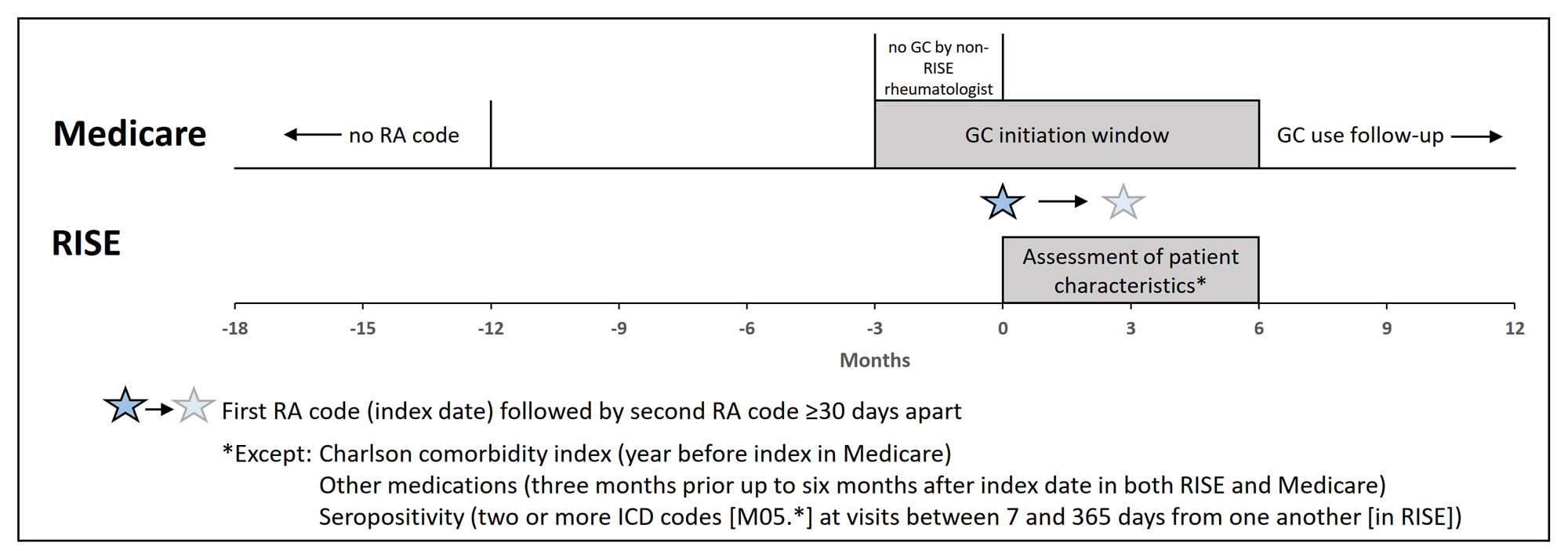
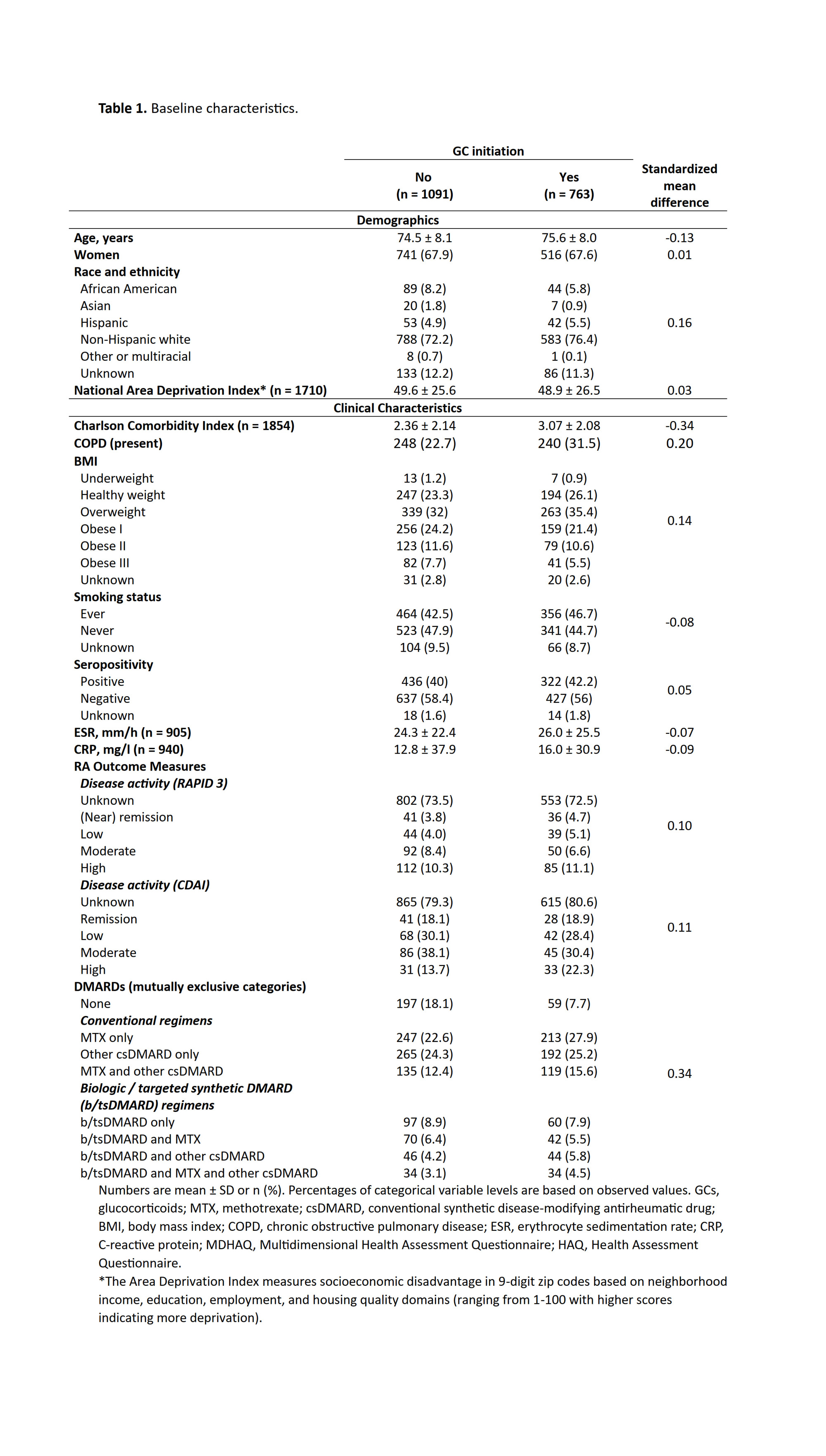
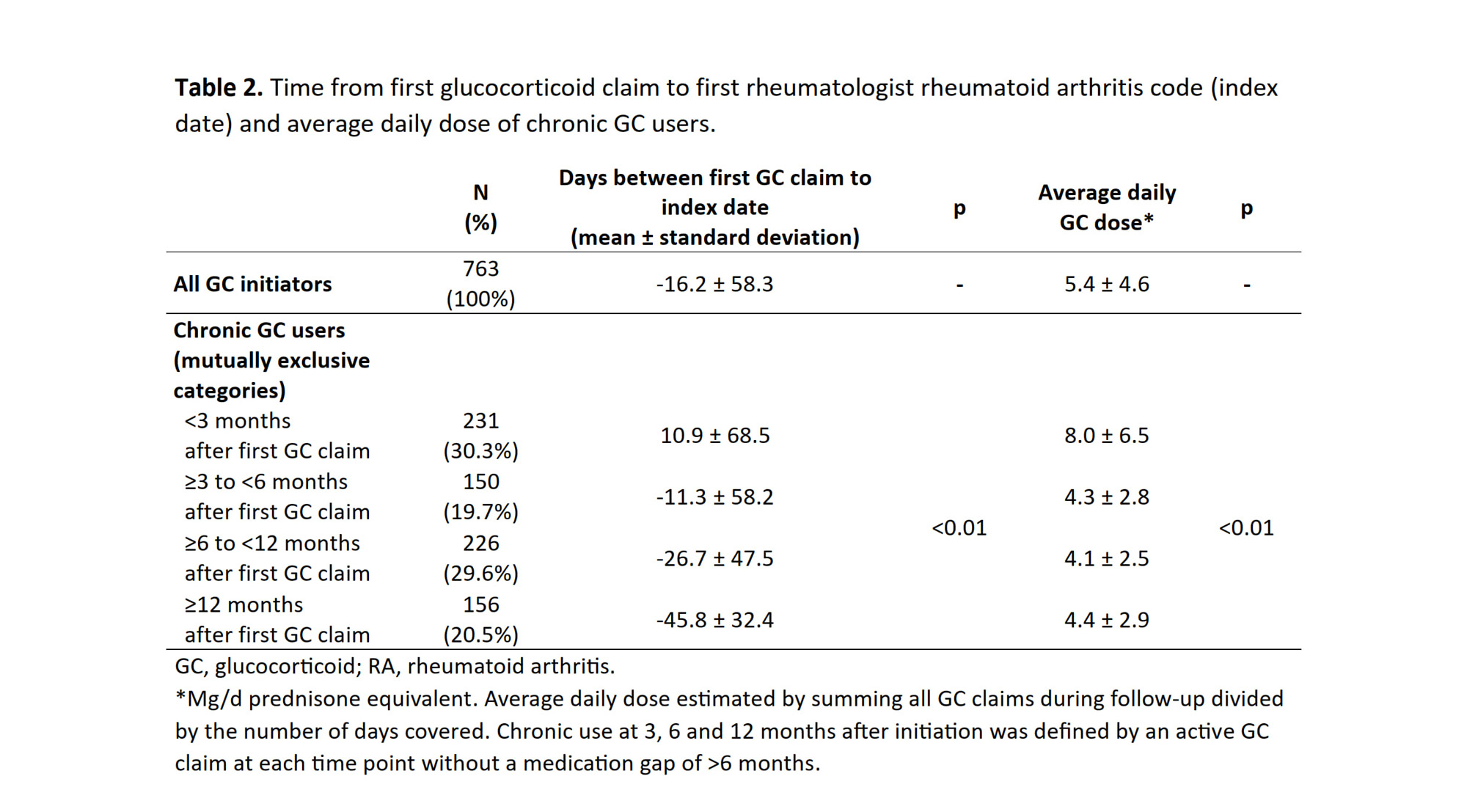
Methods: We joined data from the Rheumatology Informatics System for Effectiveness (RISE) with Medicare claims (2016-2018). Early RA patients were identified with a first RA ICD code in RISE between 01/01/2017 and 09/01/2018 (index date) plus a second code ≥30 days later. To ensure observability, we required continuous enrollment in Medicare in the year of their first RA code and the preceding year. To identify early RA patients, we required ≥18 months of observation in Medicare prior to the index date and no RA code for >12 months before the index date. Patients who received GCs before the index date from rheumatologists not participating in RISE were excluded. Patient characteristics were assessed during the six months following the index date. GC initiation for early RA was defined by a GC claim in Medicare between 3 months before to 6 months after the index date (Figure). Chronic use at 3, 6 and 12 months after initiation was defined by an active GC claim at each time point without a medication gap of >6 months. We used standardized mean differences to compare patient characteristics among GC initiators vs. non-initiators. Time between GC initiation and the start of rheumatology care was calculated as the difference between the GC initiation date and the index date. Mean GC doses during follow-up were estimated by summing total GC dose dispensed over total number of days covered. ANOVA was used to test differences in GC doses and time of GC initiation between patients with different durations of use.
Results: 1854 patients (68% female; mean [SD] age of 75 [8]) with early RA were included, of which 41% initiated GCs. GC initiators and non-initiators were similar in most baseline characteristics (Table 1), although data on disease activity was scarce. 65.1% of GC initiators had their first GC claim before the index date (mean [SD] time from first GC claim to index date: -16.2 [58.3] days). Of 497 patients with a GC claim before the index date, 63.6% received their first prescription from a non-rheumatologist. Among 763 GC initiators, 69.7%, 49.9%, and 20.5% became chronic GC users at 3, 6 and 12 months after their first GC claim. Longer duration of GC use was associated with a longer time between the first GC claim and the index date (Table 2). Mean GC doses during follow-up were less than 5 mg/d prednisone equivalent for chronic 6- and 12-month users.
Conclusion: Almost half of elderly early RA patients received GCs for their RA, most often prior to the first visit with a rheumatologist. Among patients who initiated GCs, 20% continued to receive them 12 months later. Most of the time doses were low. Initiatives to reduce GC exposure among patients with early RA will likely require close collaboration between rheumatologists and primary care to expedite referrals to rheumatology care.
To cite this abstract in AMA style:
Palmowski A, Roberts E, Li J, Kersey E, Stovall R, Buttgereit F, Yazdany J, Schmajuk G. Long-term Glucocorticoid Use in a Cohort of Elderly Early Rheumatoid Arthritis Patients: A Joint Analysis of Medicare and the Rheumatology Informatics System for Effectiveness (RISE) Data [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/long-term-glucocorticoid-use-in-a-cohort-of-elderly-early-rheumatoid-arthritis-patients-a-joint-analysis-of-medicare-and-the-rheumatology-informatics-system-for-effectiveness-rise-data/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-glucocorticoid-use-in-a-cohort-of-elderly-early-rheumatoid-arthritis-patients-a-joint-analysis-of-medicare-and-the-rheumatology-informatics-system-for-effectiveness-rise-data/