Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is characterized by autoantibodies to anti-modified protein autoantibodies (AMPAs) like anti-citrullinated protein antibodies (ACPA) and anti-acetylated protein antibodies (AAPA). Smoking is the most important environmental risk factor in autoantibody-positive RA and has been described to be specifically associated with AMPA-IgG. However, although smoking exerts its effect in the lungs, it is unknown whether smoking is preferentially associated with specific autoantibody isotypes, such as IgA, which would suggest a mucosal origin. Therefore, we set out to investigate if smoking is associated with AMPA of the IgA isotype in RA.
Methods: 618 RA patients from the Leiden Early Arthritis Cohort, of whom data were available on the presence of ACPA and AAPA -IgG and -IgA, and smoking were included. Current versus ever smoking data were collected at baseline using a questionnaire. The association between smoking and autoantibodies was assessed by logistic regression analysis. Next, a meta-analyses on results from systemic literature review on the association of smoking with ACPA-IgG and ACPA-IgA was performed.
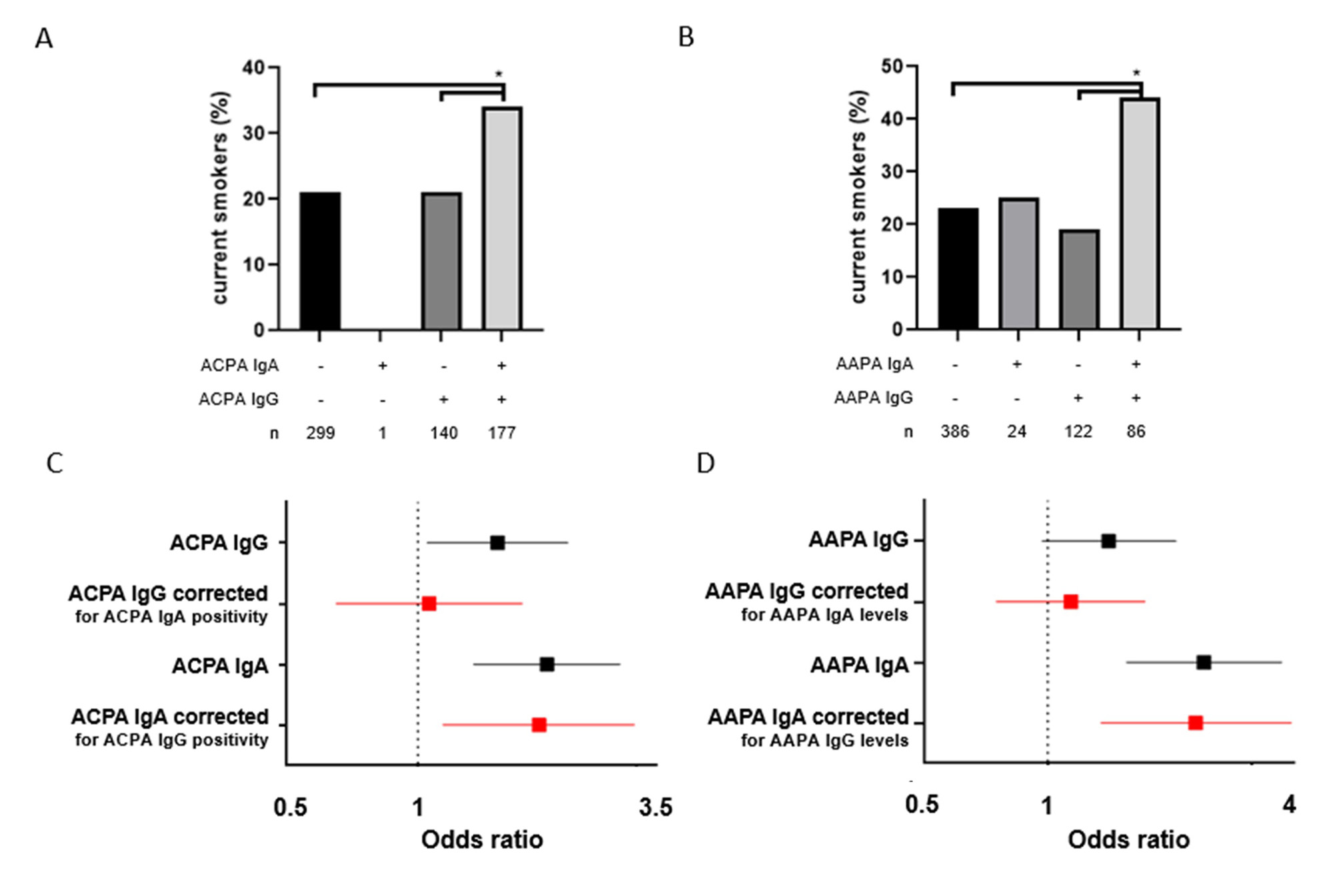
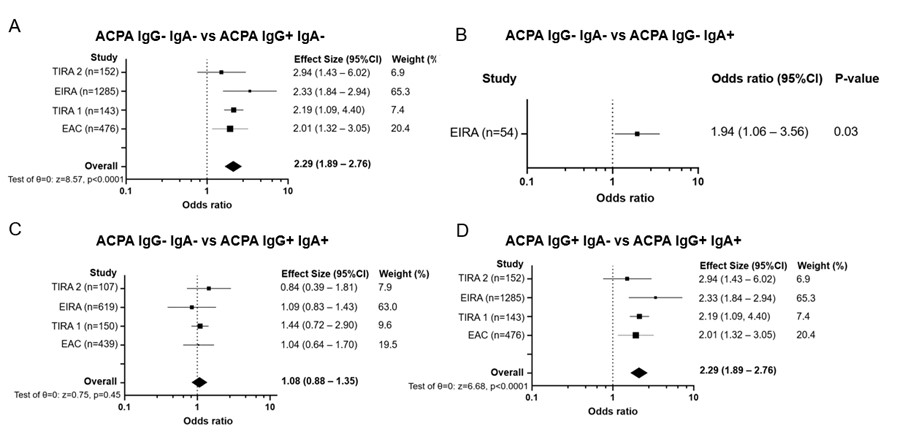
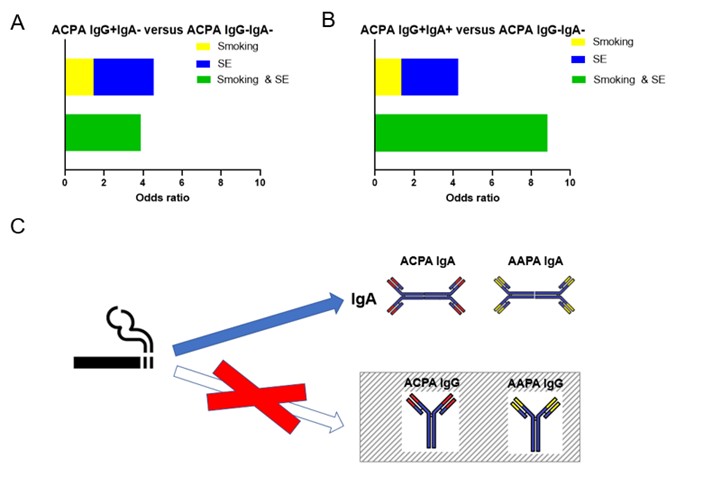
Results: In univariate analysis, smoking was associated with various autoantibodies of different isotypes (ACPA-IgG, ACPA-IgA, AAPA-IgA, RF-IgM and RF-IgA), but since isotypes often co-occur, this precluded firm conclusions. Upon examining the exact autoantibody isotype composition, smoking was only associated with AMPA-positive RA in double-positive patients, i.e. patients who harbored both IgG ánd IgA-AMPA (figure 1A and 1B). Since smoking is also associated with autoantibody levels, we then corrected the isotype-smoking associations for these levels. Strikingly, after correction for IgA, the association between AMPA-IgG and smoking was lost (Figure 1C and 1D). However, after correction for IgG, AMPA-IgA were still associated with smoking (Figure 1C and 1D).Next, a meta-analysis was performed of all publications investigating the association of smoking with ACPA-IgG and ACPA-IgA and the current data. This confirmed that smoking was associated with ACPA-IgA but not with ACPA-IgG (figure 2). Interaction analysis of shared epitope and smoking revealed that interaction was only seen in patients that were ACPA-IgG and ACPA-IgA positive, but not in patients that were only positive for ACPA-IgG (figure 3A and 3B). This indicates that the presence of ACPA-IgA is necessary for the interaction effect.
Conclusion: In RA, smoking is exclusively associated with IgA autoantibodies against post-translationally modified proteins (AMPA), and not with AMPA IgG (figure 3C). Interaction between shared epitope and smoking is also solely found in patients positive for both IgG and IgA-ACPA. These findings support the hypothesis that smoking may exert its effect by the induction of local (auto)immune responses at mucosal sites.
To cite this abstract in AMA style:
van Wesemael T, Svärd A, Dorjee A, Huizinga T, Toes R, van der Woude D. Smoking as a Risk Factor for Rheumatoid Arthritis: Exclusive Association with IgA Autoantibodies [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/smoking-as-a-risk-factor-for-rheumatoid-arthritis-exclusive-association-with-iga-autoantibodies/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/smoking-as-a-risk-factor-for-rheumatoid-arthritis-exclusive-association-with-iga-autoantibodies/