Session Information
Date: Monday, November 13, 2023
Title: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The aim of this study was to analyze the incidence of nervous system manifestations in a cohort of patients with Microscopic Polyangiitis (MPA) and Granulomatosis with Polyangiitis (GPA), and to identify if neurological manifestations influence the overall survival rates in these patients. We also evaluated how other clinical characteristics of AAV patients correlated with the neurologic involvement.
Methods: This is a retrospective single-center cohort study of AAV patients. Medical records of all patients with ANCA-positive serology from 08/2/2014 to 8/7/2021 were analyzed. One hundred and fifty one patients met the 2022 ACR/EULAR classification criteria for either MPA or GPA. An additional 19 patients with limited GPA were diagnosed but not included in this analysis. Data were collected from medical records and analyzed for organ involvement, neurologic manifestations, laboratory findings, electrophysiology and imaging.
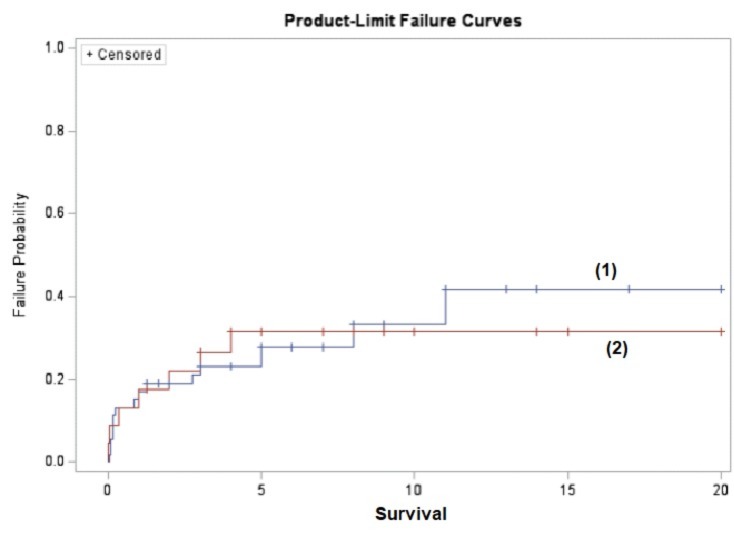
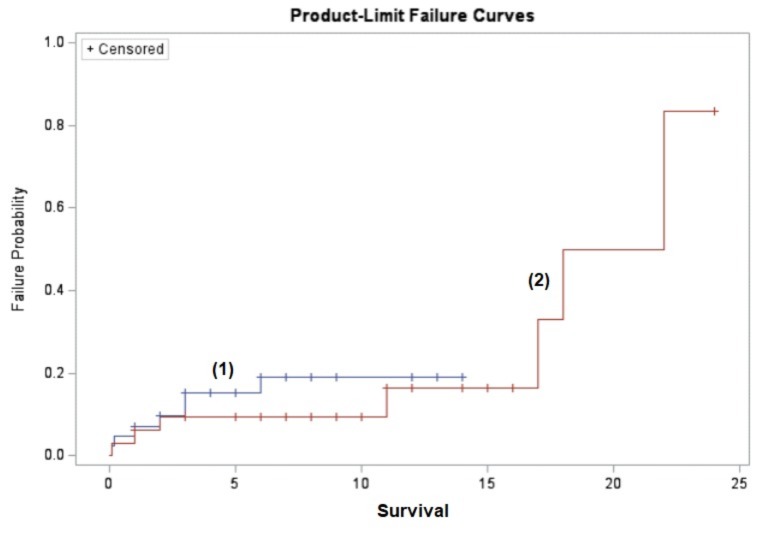
Results: One hundred and seventy patients with ANCA associated systemic vasculitis were identified. Of this number, 75 patients were diagnosed with MPA and 76 patients were diagnosed with GPA. The median duration of follow-up was 6.3 years. The majority of the MPA patients were female (60.5%) with a mean age of 58.0 years. GPA patients were mostly male (58.7%) with a mean age of 54.2 years. Each ANCA vasculitis group was analyzed separately as well as cumulative analysis was also completed. A total of 30.3% of MPA- and 44.0% of GPA-patients had neurological involvement. Peripheral neuropathy was the most common neurologic manifestation noted in 60.9% of those with evidence of neurologic involvement in the MPA group. On the contrary, the central nervous involvement was more common in the GPA group with 54.4% involvement. In the GPA cohort, the estimated cumulative survival at 1 year point in patients with neurological involvement was 82.6% in comparison to those without neurologic involvement (83.0%). In the MPA cohort, survival rate was 93.9% in those with neurologic involvement in comparison to those without neurologic involvement (92.9%). The 5-year survival in the MPA group was comparable between those with neurologic involvement (73.6%) and those without neurologic involvement (69.6%). Interestingly, patients with GPA showed a trend towards reduced overall 5-year survival rates in those without neurologic involvement (85.7%) to those that had neurologic involvement (90.9%). Analysis of secondary outcomes showed that the patients with peripheral neurologic involvement were statistically less likely to develop rapidly progressive renal disease, 29.4% vs 63.8% in the GPA group (p value=0.02) while this difference didn’t reach statistical significance in the MPA group (50.0% vs 69.4%, p value=0.22).
Conclusion: Neurologic manifestations commonly accompany systemic vasculitis such as ANCA-associated vasculitis. Nervous system involvement causes increased morbidity and reduces the quality of life in patients with either MPA or GPA but does not affect the overall survival rate at either 1 year or 5-year point in these patients. Interestingly, GPA patients with peripheral nervous system involvement were less likely to develop rapidly progressive glomerulonephritis.
(1) Represents those without neurologic involvement
(2) Represents those with neurologic involvement
(1) Represents those without neurologic involvement
(2) Represents those with neurologic involvement
To cite this abstract in AMA style:
Gheriani G, Lenert P. Neurologic Involvement Does Not Affect Cumulative Survival Rates in Patients with ANCA-associated Vasculitis and Is Less Commonly Associated with Rapidly Progressive Glomerulonephritis in Patients with GPA [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/neurologic-involvement-does-not-affect-cumulative-survival-rates-in-patients-with-anca-associated-vasculitis-and-is-less-commonly-associated-with-rapidly-progressive-glomerulonephritis-in-patients-wit/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neurologic-involvement-does-not-affect-cumulative-survival-rates-in-patients-with-anca-associated-vasculitis-and-is-less-commonly-associated-with-rapidly-progressive-glomerulonephritis-in-patients-wit/