Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: African-American (AA) ethnicity is a known predisposing factor for childhood onset systemic lupus erythematosus (cSLE) and a predictor of poor outcomes. In addition to ethnicity, income and geographical location are known drivers of health care disparities in cSLE. Despite this knowledge, there is lack of literature describing demographic and clinical features of cSLE in a predominant AA cohort. This study aims to characterize demographic and clinical features of cSLE patients in the Southeast United States (US) compared to current literature describing predominantly Caucasian cohorts.
Methods: Cross sectional study of cSLE patients from 2 centers in Southeast United States – University of Mississippi Medical center (UMMC) and University of Alabama at Birmingham (UAB). Prevalent and incident patients with cSLE at UMMC were consented for the study. Demographic, social and clinical data was retrospectively collected by chart review. Similar data was obtained for the cSLE UAB cohort via the CARRA registry database. Data from both cohorts was combined and analyzed using SPSS statistical software. Descriptive statistics were used for demographic and clinical features. Unpaired t test and chi square test were used to compare outcomes in this cohort with those reported in the literature.
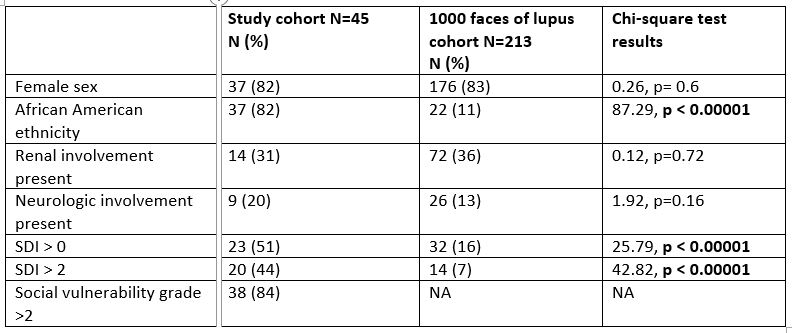
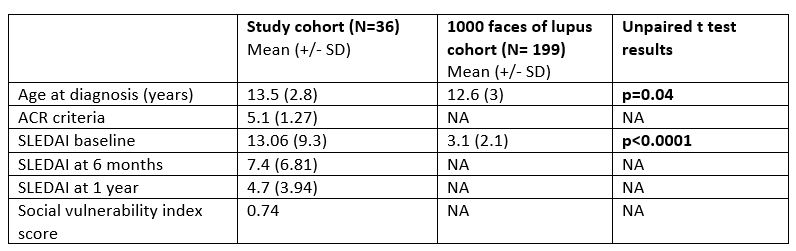
Results: Results are described for a total cohort of 45 patients, comprising 26 from UMMC and 19 from UAB. 37/45 (82.2%) were female, 37/45 (82.2%) were of AA ethnicity, and 30/45 (66.7%) had Medicaid insurance. Mean age at diagnosis (+/- SD) of SLE for the cohort was 13.5 years (+/- 2.8). Mean ACR score at diagnosis was 5.1 (+/- 1.27), SLICC score was 8.4 (+/- 2.5). Average baseline SLEDAI score was 13.06 (+/- 9.3), while SLEDAI score at 6 months and 1 year respectively were 7.4 and 4.7. Average distance traveled to see a rheumatologist was 74.83 miles compared to a national average of 42.8 miles. 37/45 patients (82%) belonged to medium-high or high Social Vulnerability Index (SVI) group based on zip code.
Average baseline SLEDAI compared to a multiethnic Canadian cohort with 10% black population, was significantly higher: 13.06 versus 3.1 (p < 0.0001, t=10.99). 23/45 had SDI > 0 (51.11%) versus 16% reported in the literature (p < 0.00001, chi-square 25.79). 20/45 (44.4%) had SDI >/= 2 compared to 7% reported in the literature (p < 0.00001, chi-square 42.82).
Patients from UMMC were offered depression and anxiety screening by a counselor in a multi-disciplinary clinic. 15/26 (57.7%) patients were screened with Revised Children’s Anxiety and Depression Scale (RCADS). 5/15 (33.3%) and 6/15 (40%) had elevated scores for depression and anxiety respectively.
Conclusion: Compared to multiethnic cohorts of cSLE from Canada, this predominantly AA patient population from two centers in the Southern United States has significantly higher disease activity and greater damage accrual. Social risk factors for this population include a higher SVI, longer distance from an academic pediatric rheumatology center and having Medicaid insurance. The effect of these factors on disparity of disease outcomes needs to be further explored with larger cohorts.
To cite this abstract in AMA style:
Dhanrajani A, Long T, Hagwood S, Karlson C, Foreman C. Characterizing Lupus in African American Children in Southern United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/characterizing-lupus-in-african-american-children-in-southern-united-states-2/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-lupus-in-african-american-children-in-southern-united-states-2/