Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: STING-associated vasculopathy with onset in infancy (SAVI) is characterized by systemic inflammation, skin vasculopathy and interstitial lung disease. However, since the initial description knowledge and clinical spectrum of this disease has substantially broadened. Here we present the clinical and laboratory characteristics of 2 families with SAVI presenting with autoimmunity and lung disease without significant cutaneous vasculopathy
Methods: We performed a retrospective chart review of patients with a genetic diagnosis of SAVI followed at the Rheumatology division of Cincinnati Children’s Hospital Medical Center (CCHMC). We collected demographic, clinical, laboratory and radiological information.
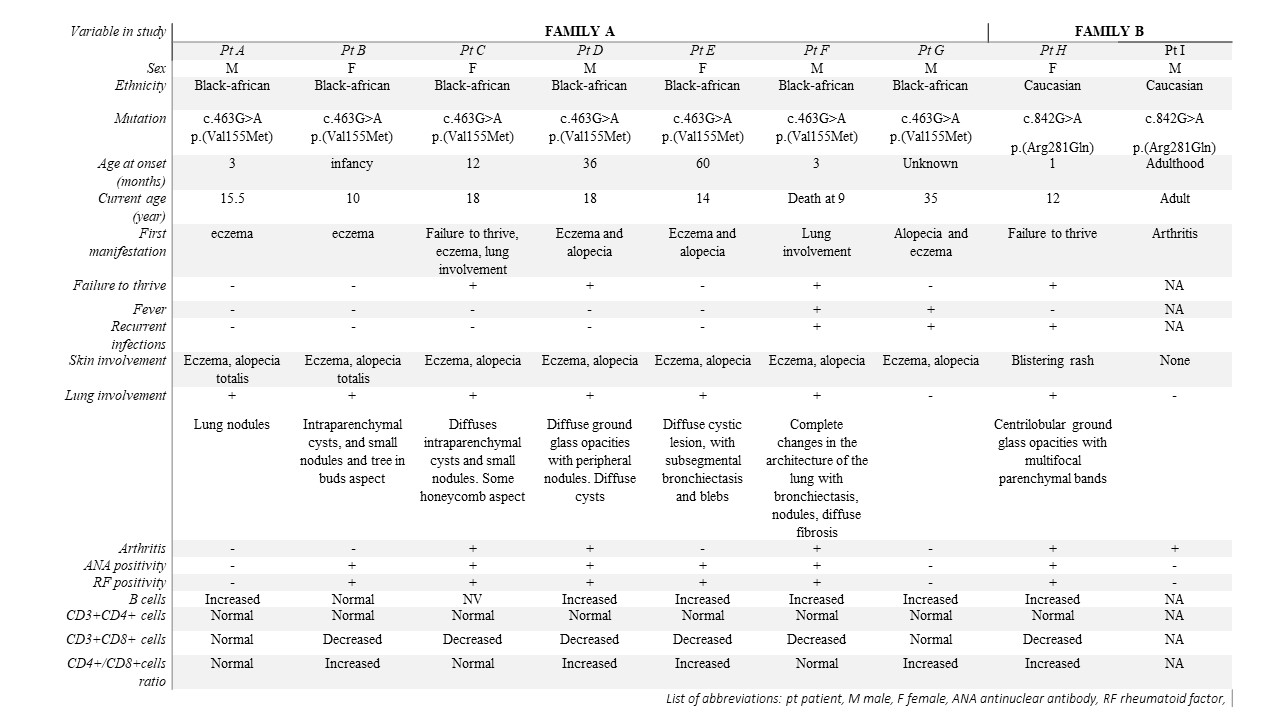
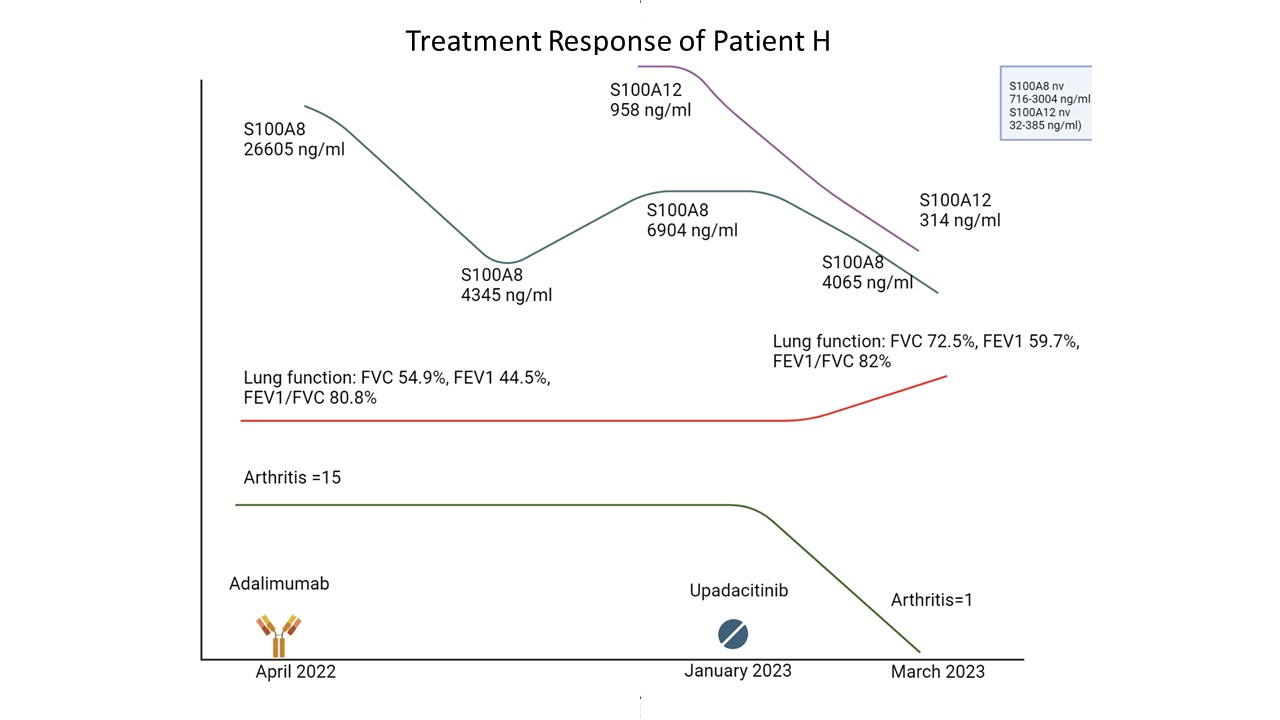
Results: We identified 9 patients from 2 families. Family A consisted of 7 individuals (the father (patient G), 3 sons and 3 daughters) carrying the heterozygous variant in STING1 c.463G >A, previously reported as cohort with undiagnosed interstitial lung disease, arthritis, and atopic dermatitis. The diagnosis was confirmed reviewing their medical records and performing genetic testing for SAVI. Family B consisted of 2 individuals (father (patient I) and daughter (patient H)), carrying the c.842G >A variant (see table 1). The median age at onset of symptoms in these 9 patients was 18 months (range 1-adulthood). The first symptom was eczema in 5 (55.5%), lung disease in 3 (33.3%), failure to thrive in 2 (22.2%), and arthritis in 1 (11.1%). Eight patients showed skin involvement (7 eczema and alopecia and 1 blistering rash), 7/9 lung involvement, 5/9 arthritis, 7/9 arthralgia and 1/9 increased liver enzymes. Seven patients underwent to lung CT that showed an interstitial lung disease of different severity characterized by minimal ground glass or nodular lesion up to diffuse cystic lesions to complete disruption of parenchyma. Lung biopsy performed in 5 patients showed chronic inflammatory bronchiolitis. Laboratory tests were available in 8 patients: all had increased ESR, 75% ANA and rheumatoid factor positivity, and 62.5% hypergammaglobulinemia. Lymphocyte subset showed expanded B cells in 75% (median 38.5% Range 31-53%), with decreased CD8+T in 71% (median 14%, R 10-38%) and 57% with increased CD4+/CD8. Plasma cytokines performed in 7 patients, showed increased value of IL1b (1/7), IL2 (2/7), IL4 (2/7), IL5 (4/7), IL8 (3/7) IL6 (5/7), TNFa (4/7). One patient of Family A died at age 9 years because of lung disease. The daughter of family B (patient H), after failing anti-TNF, received a JAK-inhibitor upadacitinib, with resolution of arthritis and improvement of lung function (spirometry) after 1.5 months of treatment.
Conclusion: The phenotype of SAVI may be extremely variable even within the same family. It is essential to reconsider prior cases with familial ILD and autoimmunity in order to identify the correct diagnosis and tailored treatment.
To cite this abstract in AMA style:
Maccora I, Vega-Fernandez P, Risma K, Schulert G. Obvious Only in Retrospect: A Cohort of STING Associated Vasculopathy in Infancy (SAVI) Without Typical Rash [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/obvious-only-in-retrospect-a-cohort-of-sting-associated-vasculopathy-in-infancy-savi-without-typical-rash/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/obvious-only-in-retrospect-a-cohort-of-sting-associated-vasculopathy-in-infancy-savi-without-typical-rash/