Session Information
Date: Monday, November 13, 2023
Title: (1155–1182) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Idiopathic Inflammatory Myopathies (IIM), collectively known as myositis, are heterogeneous disorders characterized by muscle weakness and muscle inflammation. ACR/EULAR classification criterion for IIM was published in 2016 that showed the sensitivity and specificity for probable diagnosis 87%/82% without biopsies, and 93%/88% with biopsies. The criteria is currently being used in most clinical trials and research studies. However, it has been criticized for its lack of a full panel of autoantibodies as well as the non-inclusion of other Dermatomyositis-specific rashes. The aim of our study was to evaluate if the addition of other myositis-specific antibodies (MSAs) and/or DM rashes other than Gottron papules/sign or heliotrope rash would improve the accuracy of the criteria.
Methods: Data were obtained from a prospectively collected myositis registry at a single tertiary care center but retrospectively extracted in subjects with an initial visit between 1995 to 2020. The classification criteria dataset included all variables of 2017 EULAR/ACR as well as Bohan and Peter myositis classification criteria.Additional variables were verified by chart review if/when required and all variables and scores were cross-checked by 2 physicians. Classification scores were re-calculated by adding:
- all non-Jo1 MSA/MAA receiving the same score as Jo-1,
- all other DM rashes except Gottron papule/sign, and heliotrope (i.e., shawl sign, V-neck, holster sign, malar rash not sparing nasolabial fold, mechanics hands, periorbital edema) receiving the same score as Gottron papules.
- both a & b.
Psychometric properties of the 2017 EULAR/ACR classification criteria and proposed modifications were calculated using the diagnosis made by expert rheumatologist physicians as the gold standard.
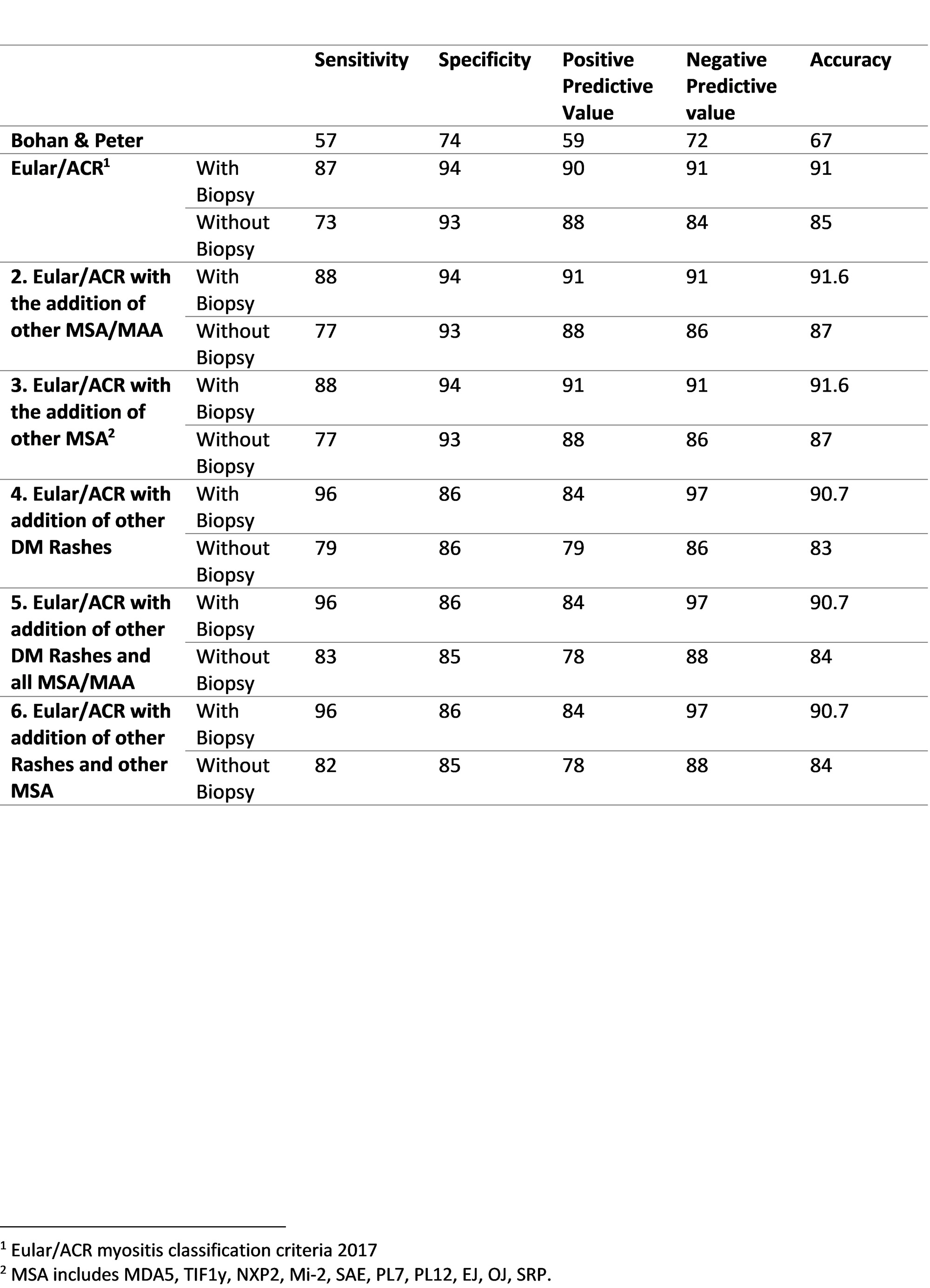
Results: 798 patients with IIM including 268 with dermatomyositis, 41 with clinically amyopathic dermatomyositis (CADM). In our analysis, 2017 EULAR/ACR showed 91% accuracy, with high sensitivity (87% and 73%) and specificity (94%, and 93%), with and without muscle biopsy, respectively. Bohan and Peter showed lower sensitivity and specificity of 57% and 74% respectively.
The modification of adding other MSA/MAA along with Anti Jo1 leads to a minor improvement in sensitivity (88% and 77% with and without biopsy respectively) without loss of specificity. Adding other DM rashes with Gottron papules increases sensitivity significantly (96% and 79% with and without biopsy, respectively) but with a decrease in specificity (86%). (Table 1)
The modification of adding other MSA/MAA as well as other DM rashes together improves sensitivity the best but at the cost of specificity.
Conclusion: The addition of other skin rashes and/or MSA to the 2016 EULAR/ACR criteria improves sensitivity but at a cost of specificity. Modification of the EULAR/ACR classification criteria is required to overcome some of the shortcomings of the current criteria.
To cite this abstract in AMA style:
Hasan Y, Chung K, Ascherman D, Moghadam-Kia S, V. Oddis C, Aggarwal R. Inclusion of All Myositis Specific Autoantibodies or Other Rashes Leads to Better Sensitivity but Lower Specificity of 2017 EULAR/ACR Myositis Classification Criteria for Dermatomyositis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/inclusion-of-all-myositis-specific-autoantibodies-or-other-rashes-leads-to-better-sensitivity-but-lower-specificity-of-2017-eular-acr-myositis-classification-criteria-for-dermatomyositis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inclusion-of-all-myositis-specific-autoantibodies-or-other-rashes-leads-to-better-sensitivity-but-lower-specificity-of-2017-eular-acr-myositis-classification-criteria-for-dermatomyositis/