Session Information
Date: Monday, November 13, 2023
Title: (1124–1154) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Polymyalgia rheumatica (PMR) treatment is primarily based on long-term corticosteroids, which results in significant toxicities. Studies1,2 have shown that patients with PMR are exposed to years of corticosteroid treatment. In a single academic center cohort, we found that 76% of patients remained on steroids at the end of two years.3 In a second cohort of PMR patients, we explored the baseline characteristics and established the success rate in discontinuing steroid treatment at years one and two after initiating the treatment.
Methods: A retrospective observational study was conducted using data collected from a rheumatology clinic at an academic Medical Center. We included patients with a primary diagnosis of PMR or PMR associated with Giant cell arteritis (GCA) and a minimum of 1-year follow-up. Patients with other rheumatological disorders were excluded. Out of 403 PMR charts reviewed from 2011 to 2021, 346 patients met the inclusion criteria.
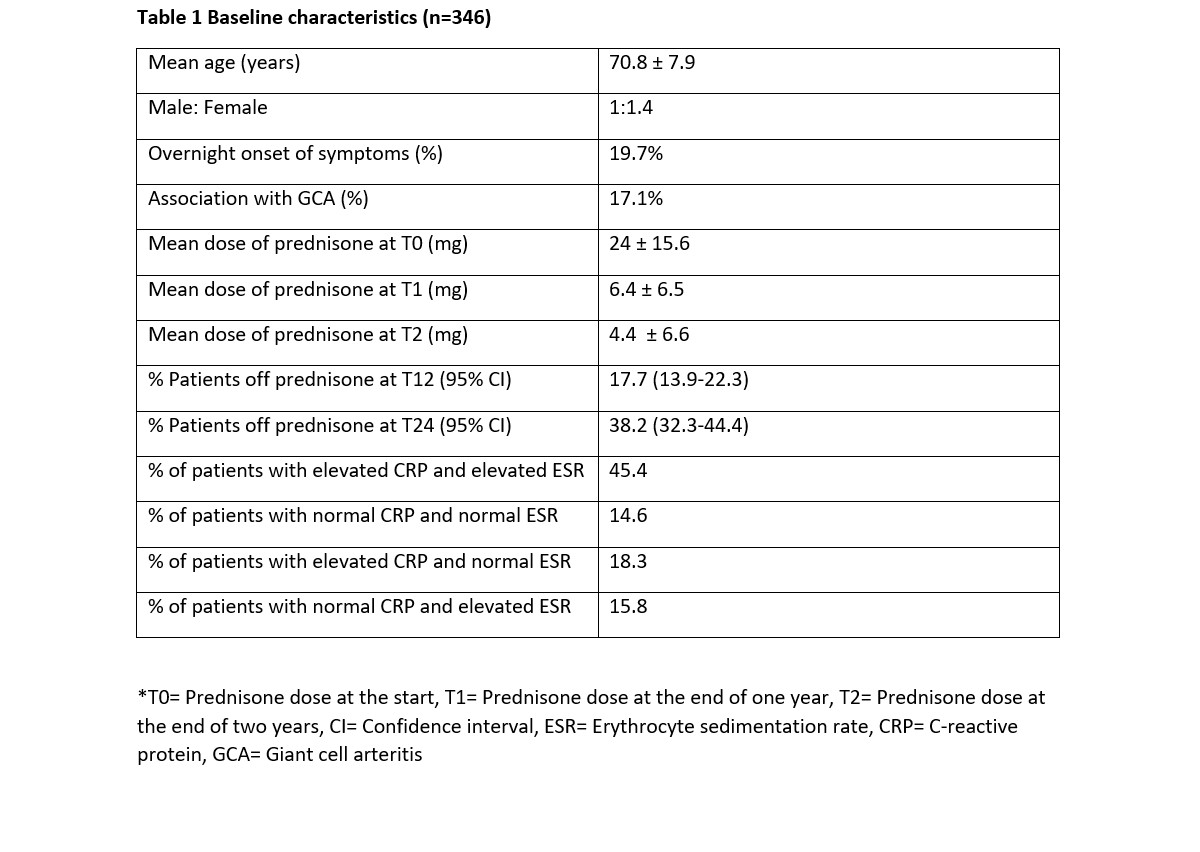
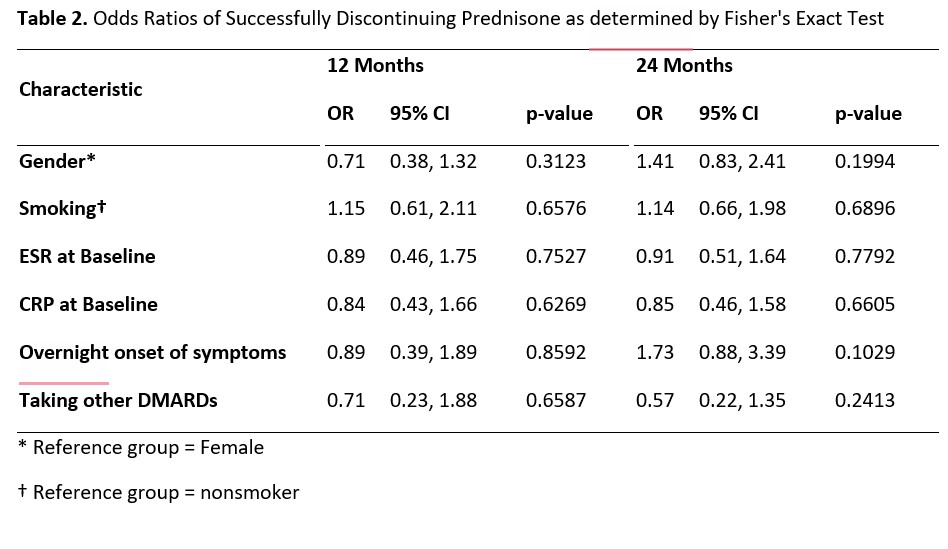
Results: The mean age of the patient population was 71 years, with 59% being females and 41% males. Approximately 20% of the patients experienced an abrupt onset of symptoms. Among the PMR patients, 17.1% had a concurrent diagnosis of GCA, which usually developed alongside or after the PMR diagnosis. Only 2% of patients presented with Remitting Seronegative Symmetrical Synovitis with Pitting Edema (RS3PE). At the beginning of treatment (T0), the mean prednisone dose was 24 mg daily. At one year (T1), it decreased to 6.4 mg, and at two years (T2), it further reduced to 4.3 mg daily. At the end of one year, 17.7% of patients had discontinued prednisone, while only 38% had achieved discontinuation by the end of two years. The majority of patients exhibited elevated markers of inflammation (ESR or CRP), with only 14.6% presenting with normal values initially. The only patient characteristic associated with successful discontinuation was the initial steroid dose. Multivariable logistic regression analysis showed that with each unit increase in the initial prednisone dose, the odds of successfully discontinuing prednisone at 12 months decreased by 3% (p = 0.034). However, the significance of this association was not sustained at the 24-month mark. No other baseline characteristics were associated with successful prednisone discontinuation.
Conclusion: The clinical course of PMR is characterized by prolonged corticosteroid use, with a discouraging rate of successful prednisone discontinuation. Our study validates previous observations3 and provides additional insights into the clinical characteristics of PMR patients. Similar to prior research4,5, our study demonstrates that the initial corticosteroid dosage predicts the likelihood of successful discontinuation. However, the significance of this association diminishes at the 24-month mark, highlighting the need for further investigation. We acknowledge the limitations of our retrospective study, including potential selection bias due to the inclusion of patients with only one year of follow-up. Nonetheless, these findings underscore the urgency for additional research to identify and incorporate alternative disease-modifying anti-rheumatic drugs (DMARDs) into the PMR treatment regimen.
To cite this abstract in AMA style:
Rigby W, Mackenzie T, Campbell E, Skydel J, Savage B, Dimambro M, Tiwari V. Exploring the Clinical Characteristics and Correlation with Corticosteroid Dependence in Polymyalgia Rheumatica (PMR) Patients: Insights from an Academic Center [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/exploring-the-clinical-characteristics-and-correlation-with-corticosteroid-dependence-in-polymyalgia-rheumatica-pmr-patients-insights-from-an-academic-center/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploring-the-clinical-characteristics-and-correlation-with-corticosteroid-dependence-in-polymyalgia-rheumatica-pmr-patients-insights-from-an-academic-center/