Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) is the most common cause of kidney injury in patients with systemic lupus erythematous (SLE) and is associated with higher morbidity and mortality. Low adherence to treatment regimens is common amongst patients with LN and is correlated with high rates of relapse, increased hospitalizations, and poor renal outcomes. Our objective was to assess and identify barriers to medication adherence for our patients with LNon mycophenolate mofetil (MMF).We used this data to design targeted interventions aimed at improving medication adherence for our patients with LN on MMF in our large integrated health system at Kaiser Permanente Oakland Medical Center, California.
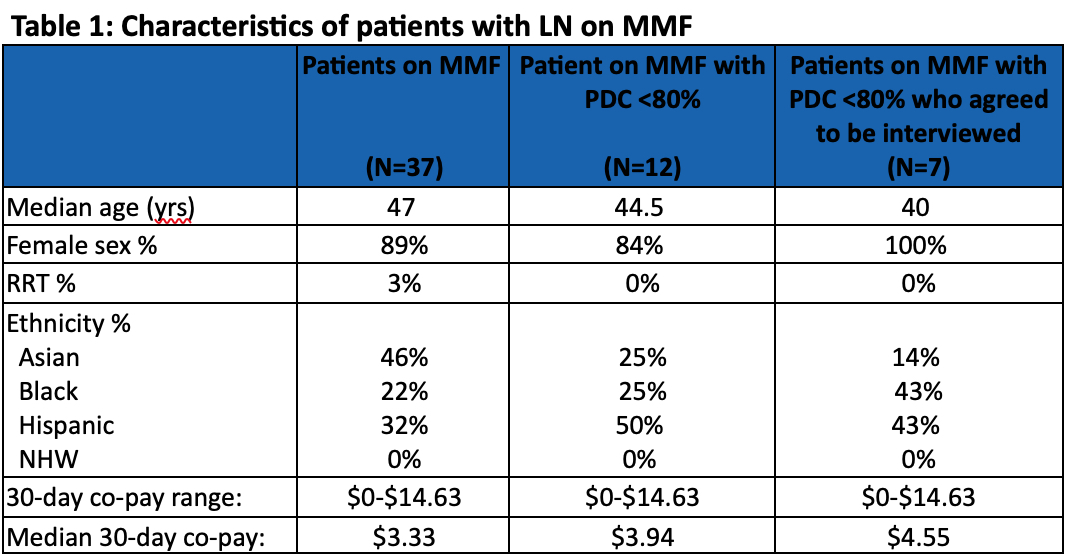
Methods: We identified patients with a diagnosis of LN, who were taking MMF between 11/30/21 and 11/30/22. We collected demographic information including age, gender, 30-day copay, ethnicity, requirement of renal replacement therapy, and proportion of days covered (PDC) for MMF. We identified patients with a PDC of less than80% and surveyed them for barriers to medication adherence. Our survey questions sought to elucidate barriers such as medication side effects, cost, refill processes, and lab draws. We also asked open-ended questions to gain insight into how SLE has affected their lives.
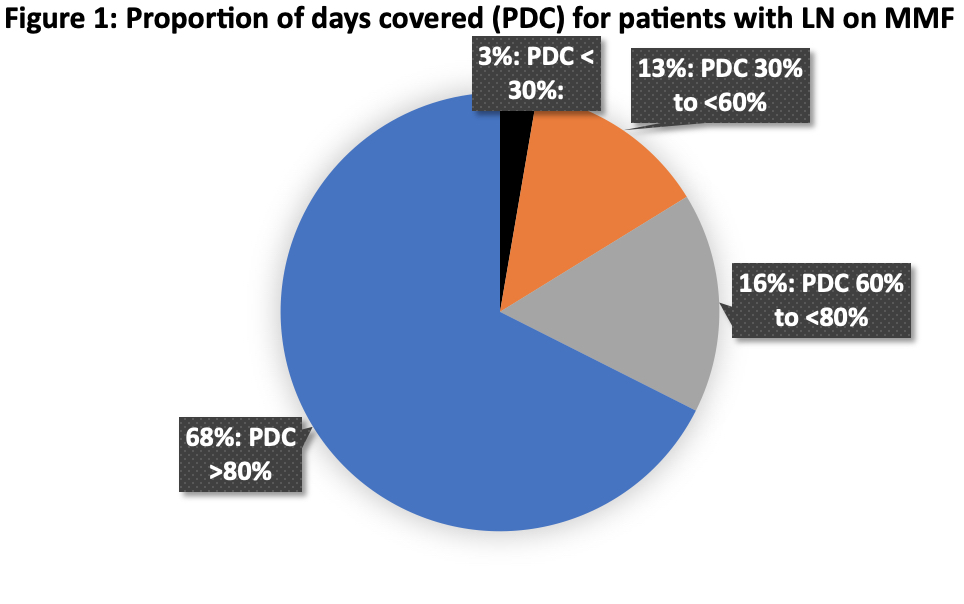
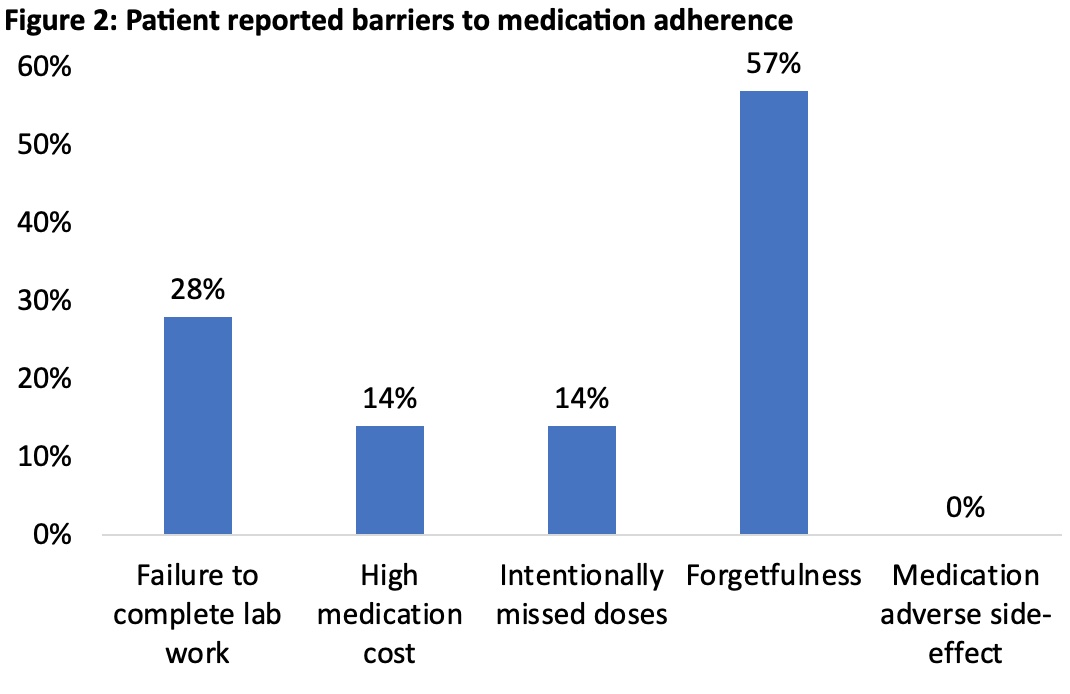
Results: Of 37 patients with LNon MMF, almost a third (12/37) had PDC less than 80%. More than half (7/12) of these patients agreed to be interviewed. They identified the following barriers to medication adherence: forgetfulness57% (4/7), incompletelabwork28% (2/7),medication cost 14% (1/7),and intentionally missed doses 14% (1/7). No patients identified medication side effects as a barrier. More than two thirds (5/7) reported no issues with obtaining new prescriptions from the pharmacy. The median 100-day co-pay for MMF was $13.13 and 2/7 (28%) patients paid $0 for their medications.
Conclusion: At KP Oakland, two thirds of our patients with LNare adherent to their MMF; forgetfulness appears to be a challenge for our non-adherent patients. The next steps to our quality improvement initiatives will focus on the following: 1) patient and provider education about tools (medication and lab reminder apps) to promote medication adherence and 2) creating a multidisciplinary rheumatology and nephrology committee to identify and discuss patients with LN who are at risk of disease progression.
To cite this abstract in AMA style:
Macko C, Chen P, Santos R, Ramalingam N, Tran N, Zheng S. “Lupus Doesn’t Have Me, I Have Lupus” a Patient Centered Quality Improvement Project to Increase Medication Adherence for Patients with Lupus Nephritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/lupus-doesnt-have-me-i-have-lupus-a-patient-centered-quality-improvement-project-to-increase-medication-adherence-for-patients-with-lupus-nephritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-doesnt-have-me-i-have-lupus-a-patient-centered-quality-improvement-project-to-increase-medication-adherence-for-patients-with-lupus-nephritis/