Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with SLE experience increased all-cause mortality and have a higher risk of hospitalization than the general population. Recently the classification criteria for SLE were updated resulting in an additive score to classify patients with SLE.
A higher score (≥20) in this classification criteria has been associated with disease severity in populations from referral centers (susceptible to referral bias), but this strategy has not been explored in a community setting. We aimed to assess the utility of the 2019 SLE classification criteria score for predicting mortality and hospitalizations in a population-based cohort of patients with recent SLE classification.
Methods: All incident patients meeting the 2019 EULAR/ACR SLE classification criteria in a population-based cohort between 1976-2018 were included. The EULAR/ACR SLE criteria components were abstracted by retrospective review of medical charts. We used EULAR/ACR score at 1 year from meeting classification. We evaluated the association between a score ≥20 points and mortality and the first unplanned hospitalization using Cox proportional hazards models adjusted for age, sex, and calendar year. Hospitalization data was available starting in 1995, and only incident patients after this were included in the hospitalizations analysis. Additionally, we re-fit multivariable models with EULAR/ACR score included as a penalized spline to explore possible non-linear relationships with outcomes and assess potential cut-off points. Patients were followed until March 2022, death, or lost to follow-up. A p-value < 0.05 was considered statistically significant.
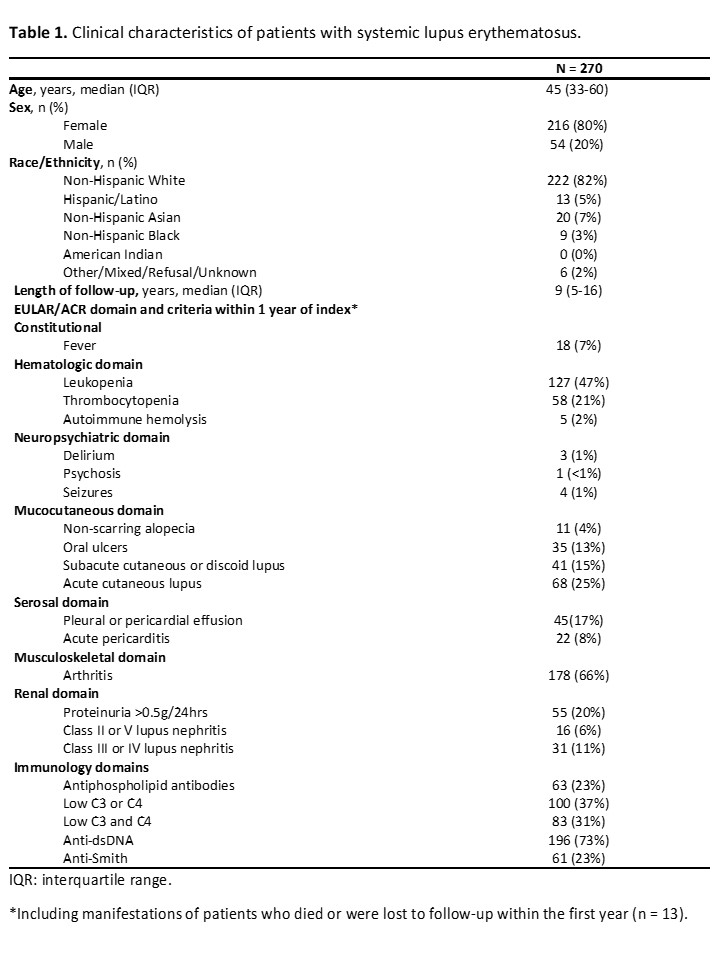
Results: We included 270 patients with SLE. The median age was 45 (IQR 33-60) years; 80% were female and 82% were non-Hispanic White. The median length of follow-up was 9 (IQR 5-16) years. The most common clinical manifestations within 1 year of index date were inflammatory arthritis (66%), leukopenia (47%), and acute cutaneous lupus (25%). 73% were anti-dsDNA positive and 20% had proteinuria (Table 1). During follow-up, 68 patients died and 122 experienced unplanned hospitalization. 38% of patients had a score ≥20 points within 1 year of index.
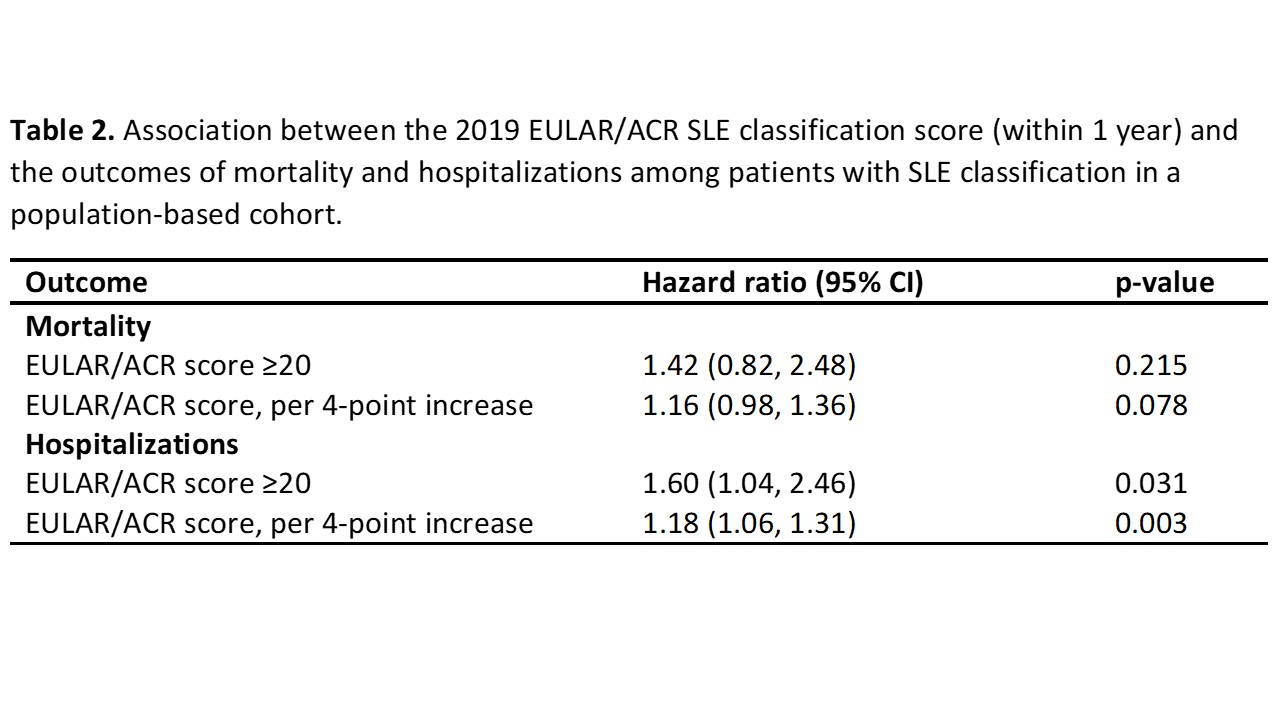
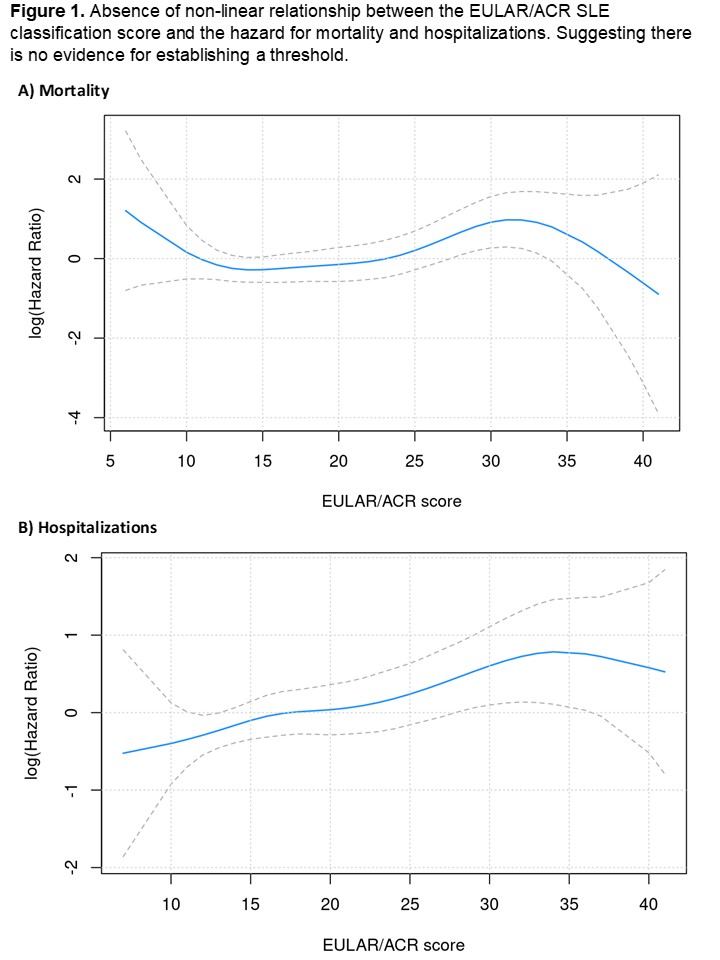
A EULAR/ACR score ≥20 points within the first year of classification were not predictive for mortality (HR 1.42, 95% CI 0.82-2.48; p=0.22) but was for hospitalizations (HR 1.60, 95% CI 1.04-2.46, p=0.031) compared to a score ≤19 points. Assessing the EULAR/ACR score as a continuous predictor, we did not find a statistically significant association with mortality (HR 1.16 per 4-point increase, 95% CI 0.98-1.36, p=0.078), however, we estimated an 18% increase in the hazard for hospitalization (HR 1.18 per 4-point increase, 95% CI 1.06-1.13, p=0.003) (Table 2). We did not find any evidence of meaningful non-linear effects between the EULAR/ACR score and mortality (p=0.075) or hospitalizations (p=0.805) that suggested another potential score threshold to test (Figure 1).
Conclusion: Among patients with recent SLE classification from a population-based cohort, the EULAR/ACR SLE classification score (≥20 points) was not a useful predictor for mortality compared to patients with SLE from referral centers, but it was predictor for hospitalizations.
To cite this abstract in AMA style:
Figueroa-Parra G, Hanson A, Sanchez-Rodriguez A, Meade-Aguilar J, Crowson C, Duarte-Garcia A. Utility of the 2019 EULAR/ACR SLE Classification Criteria Score as Predictor for Mortality and Hospitalizations in a Population-Based Cohort: The Lupus Midwest Network [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/utility-of-the-2019-eular-acr-sle-classification-criteria-score-as-predictor-for-mortality-and-hospitalizations-in-a-population-based-cohort-the-lupus-midwest-network/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/utility-of-the-2019-eular-acr-sle-classification-criteria-score-as-predictor-for-mortality-and-hospitalizations-in-a-population-based-cohort-the-lupus-midwest-network/