Session Information
Date: Thursday, March 30, 2023
Title: Plenary Abstracts Session I
Session Type: Plenary Session
Session Time: 2:30PM-3:30PM
Background/Purpose: High rates of serious infection have beenreported in pediatric systemic lupus erythematosus (pSLE), but modern care practices including pneumococcal vaccination, changing corticosteroid use, and B-cell-depletion may modify infectious risks. The current burden of infections in pSLE is unknown. We conducted a retrospective study using the Pediatric Health Information System (PHIS) to determine number and type of serious infections in hospitalized children with pSLE, and to identify risk factors for poor outcomes.
Methods: We included patients 2-21 years of age with ICD-9 or ICD-10 code for SLE (710.0, M32*) during admission to a hospital participating in PHIS, an administrative database of 50 freestanding childrens hospitals in the United States, from 2009-2021. Serious infections were identified using ICD-9 and ICD-10 codes and antimicrobial medication use. Summary statistics were used to describe demographic and disease features of the entire PHIS pSLE cohort, and the subset hospitalized with serious infection. We calculated the frequency of admission, intensive care admission, and mortality by type of infection. Logistic regression using generalized estimating equations was used to identify risk factors for ICU admission and in-hospital mortality among children hospitalized with infection.
Results: We identified 11,178 unique patients with pSLE and at least one hospitalization in PHIS. Among this cohort, there were 32,414 hospitalizations, of which 3,839 (11.8%) had codes for serious infections. Patients hospitalized with serious infections were similar in demographic and disease characteristics to the entire PHIS pSLE cohort (Table 1). Specific infections and outcomes of hospitalization are reported in Table 2. The most common infections were bacterial pneumonia (n=1159), cellulitis (n=810), sepsis (n=693) and urinary tract infections (n=498). In-hospital mortality occurred in 1% of children with pSLE hospitalized for all indications and in 3% of hospitalizations with a code for serious infection. The highest in-hospital mortality rates occurred in hospitalizations with codes for pneumocystis jirovecii pneumonia (22%), aspergillosis (15%), and other fungal infections (18%). Approximately half of children who died had ≥2 serious infections during the hospitalization in which death occurred. Lupus nephritis and end-stage renal disease (ESRD) were significantly associated with increased odds of ICU admission (OR [95% CI] of 1.6 [1.3, 1.8] and 2.1 [1.6, 2.7], respectively) and in-hospital mortality (OR [95% CI] 2.3 [1.3, 4.0] and 2.1 [1.0, 4.2]) among children admitted for a serious infection (Figure 1).
Conclusion: Hospitalizations including codes for serious infection comprised a small proportion of pSLE admissions but accounted for the majority resulting in in-hospital mortality among patients with pSLE in the PHIS cohort. While bacterial infections were more common, mortality rates of hospitalizations with codes for fungal infections were high. Patients with pSLE and renal disease were at increased risk for poor outcomes. Further research is needed to understand modifiable risk factors for infection and severe outcomes, including immunosuppressant medication use.
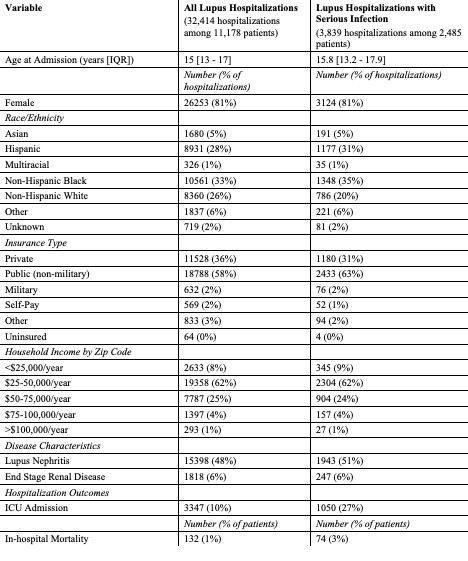 Table 1: Characteristics of children with pSLE hospitalized for any indication and with serious infection from 2009_2021
Table 1: Characteristics of children with pSLE hospitalized for any indication and with serious infection from 2009_2021
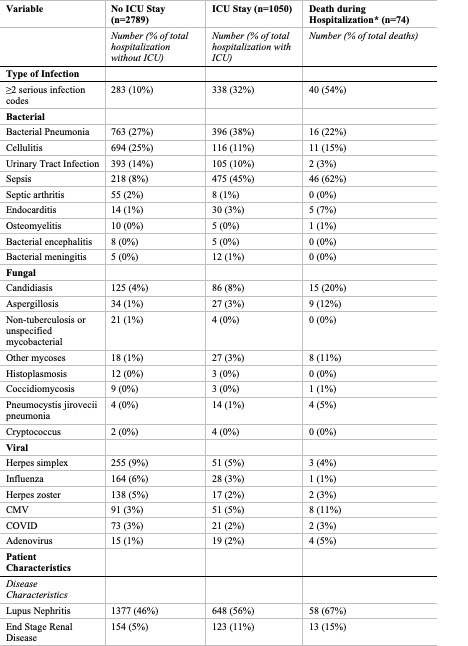 Table 2: Hospitalization Outcome by Type of Infection and Disease Characteristics
Table 2: Hospitalization Outcome by Type of Infection and Disease Characteristics
*Death during hospitalization was considered either with or without ICU admission.
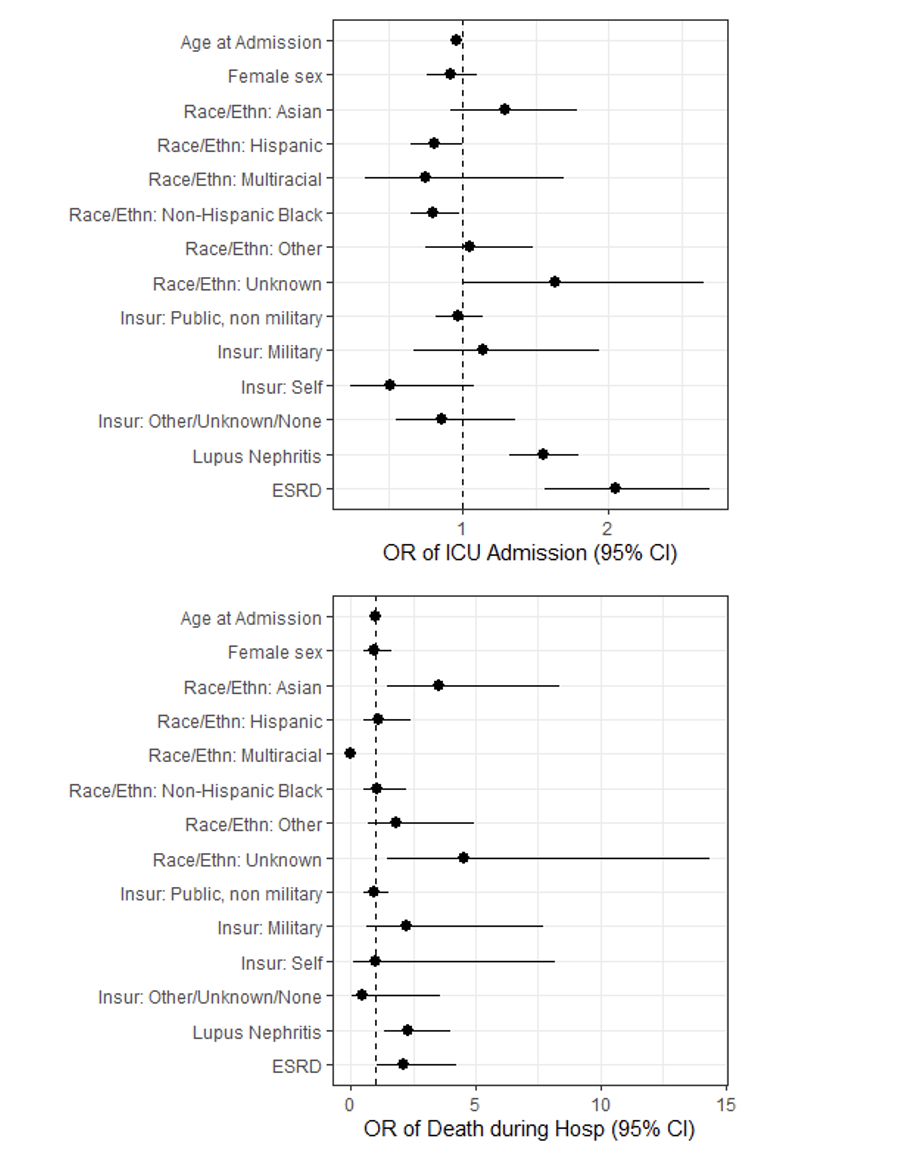 Figure 1: Odds of ICU admission and mortality among children with pSLE hospitalized with infection
Figure 1: Odds of ICU admission and mortality among children with pSLE hospitalized with infection
To cite this abstract in AMA style:
Roberts J, Faino A, Bryan M, Cogen J, Morgan E. Serious Infections Among Children with Systemic Lupus Erythematosus in the Pediatric Health Information System [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/serious-infections-among-children-with-systemic-lupus-erythematosus-in-the-pediatric-health-information-system/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serious-infections-among-children-with-systemic-lupus-erythematosus-in-the-pediatric-health-information-system/
