Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at increased risk for serious infections. Several infection risk scores have been developed over the last decade for patients with RA. These scores are largely based on a combination of patient demographics, medications, and a limited list of morbidities. Patients with RA have a higher prevalence of multimorbidity compared with non-RA patients, and some morbidities associated with the risk of infection may remain unaccounted in the existing infection risk scores. Thus, in this study we aimed to examine associations between a comprehensive list of morbidities and the risk of serious infection in patients with RA.
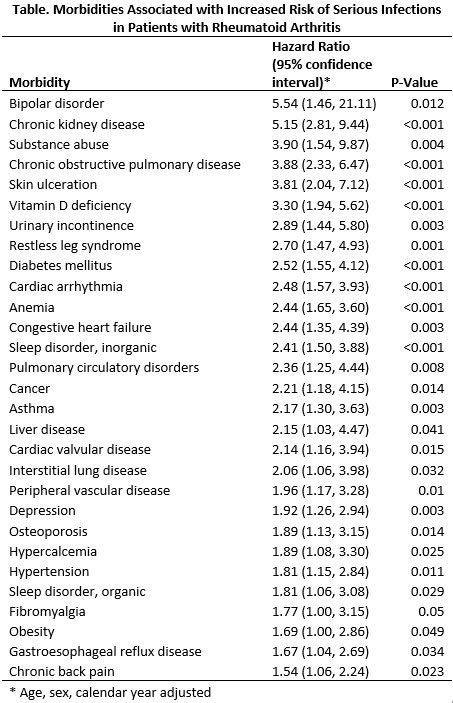
Methods: This population-based cohort study included patients from a geographically well-defined area with incident RA from 1/1/1995 through 7/1/2015 meeting the 1987 American College of Rheumatology criteria. Patients were followed until the earlier of: death, migration from the region, or 07/01/2015. Serious infections requiring hospitalization were identified using ICD-9 codes. The presence of fifty-five potential co-morbidities was then ascertained, requiring two separate ICD-9 codes at least 30 days apart. Conditional frailty models (a variation of Cox model that accounts for multiple events per patient) were used to analyze the association between each morbidity and serious infection, adjusting for age, sex, and calendar year. Hazard ratios with 95% confidence intervals (95%CI) were determined for each morbidity.
Results: There were 911 patients (70% female, mean age 56 years) who met inclusion criteria. During the 5,492 person years of observation, there were 209 serious infections resulting in an incidence of 3.8 infections per 100 person-years. One hundred and sixteen patients (13%) had at least one hospitalization for serious infection. The most common morbidities (% of patients; % person-years) included hypertension (48.4%; 38.6%), hyperlipidemia (48.1%; 34.6%), osteoarthritis (47.5%; 29.1%), and chronic back pain (46.7%; 28.1%). Twenty-nine of the 55 morbidities assessed were associated with an increased the risk of serious infection (Table). Comorbidities conferring the highest risk include bipolar disorder (HR 5.54; 95%CI 1.46 to 21.11), chronic kidney disease (HR 5.15; 95%CI 2.81 to 9.44), skin ulcers (HR 3.90; 95%CI 1.54 to 9.87), and chronic obstructive pulmonary disease (HR 3.88; 95%CI 2.33 to 6.47).
Conclusion: This population-based study highlights several morbidities associated with increased risk of serious infections in patients with RA. Future studies may aim to combine a similar comprehensive comorbidity risk profile with other known infection risk factors such as medications and smoking status to create improved predictive models for serious infection.
To cite this abstract in AMA style:
Kimbrough B, Crowson C, Lennon R, Davis J, Myasoedova E. Morbidities Associated with Serious Infections in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/morbidities-associated-with-serious-infections-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/morbidities-associated-with-serious-infections-in-patients-with-rheumatoid-arthritis/