Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Periodic Fever Syndromes (PFS) are common referrals to pediatric rheumatology clinics. While the syndrome of Periodic Fevers, Aphthous stomatitis, Pharyngitis, and Adenitis (PFAPA) is the most common PFS diagnosis in primary care clinics, patients with monogenic autoinflammatory diseases (AID) and undifferentiated PFS presentations (genotype negative) are enriched in subspecialty clinic settings. The availability of Periodic Fever Syndrome panels that screen for the most common AID gene mutations has progressively increased the number of genetic diagnoses in pediatric rheumatology over the past 2 decades. We present herein a summary of our clinic experience with a specific focus on undifferentiated PFS patients.
Methods: All PFS patients who were evaluated in our Pediatric Rheumatology clinics at least twice between July of 2005 and July of 2019 are included in this review. Genotyping prior to 2005 followed a candidate gene approach, whereas genotyping after that year included a broader panel of AID mutations in 7-12 genes (GeneDx and Invitae Labs, respectively).
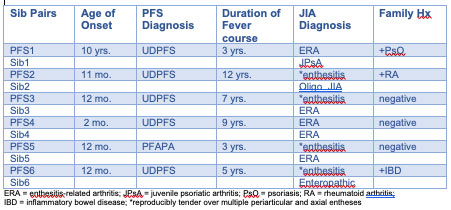
Results: 147 unique patients with periodic fever syndromes were evaluated over the course of this 14-year interval. Of these, 49 (33.1%) were classified as PFAPA without need for genotyping. 73 (49.7%) were genotyped, with 26 (35.6%) having an identified monogenic AID, while 47 (64.4%) had negative results and were assigned a diagnosis of undifferentiated PFS (UDPFS). In comparing the UDPFS patients to the PFAPA group, we found that the UDPFS group contained a higher percentage of females (62% versus 48%) and was more ethnically diverse. There was no statistical difference in age of onset, fever periodicity, duration of episodes, or time to remission. We identified a number of sibling pairs in our PFS population, and 6 pairs comprised one sib with PFS and the other with JIA; 5 out of these 6 PFS sibs were classified as UDPFS. While fevers in these UDPFS sibs remitted, all progressed to a JIA phenotype consistent with early enthesitis-related arthritis or psoriatic arthritis.
Conclusion: Within our clinic population of PFS, approximately 2/3 who were genotyped remain undifferentiated based on negative mutation screening. Of interest, some of these UDPFS patients have evolved to a JIA phenotype identical to that of their sibling. Further genotyping of these JIA sib pairs may reveal polymorphisms common to both PFS and JIA.
To cite this abstract in AMA style:
Anderson J, Bingham C, Scalzi L, Gaffney N, Hays K, Groh B, Hahn T. Prevalence and Evolution of Undifferentiated Periodic Fever Syndromes in an Academic Pediatric Rheumatology Practice [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-evolution-of-undifferentiated-periodic-fever-syndromes-in-an-academic-pediatric-rheumatology-practice/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-evolution-of-undifferentiated-periodic-fever-syndromes-in-an-academic-pediatric-rheumatology-practice/