Session Information
Date: Sunday, November 13, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Cardiovascular events occur more frequently and with earlier onset in patients with Systemic Lupus Erythematosus (SLE) compared with healthy individuals. Several studies have concluded that alteration of the immune system and cytokine axis coupled with increase in oxidative stress accelerate plaque formation and destabilization. Moreover, anti-phospholipid was also found to promote thrombosis in SLE patients. Although several studies have linked SLE with increased risk of Acute Myocardial Infarction (AMI), recent epidemiological data from large population-based studies is lacking. In our study, we aimed to analyze temporal trends and predictors associated with increased risk of hospitalizations due to AMI among SLE patients by using nationally representative dataset from the United States.
Methods: We analyzed Nationwide Inpatient Sample (NIS) and Healthcare Cost and Utilization Project (HCUP) data for years 2010-2018. Hospitalizations among adult SLE patients were identified by previously validated ICD-9/10-CM codes. Proportion of hospitalizations due to primary diagnosis of AMI was calculated. We then utilized the Cochrane Armitage trend test and multivariate survey logistic regression models to analyze trends and predictors of AMI among SLE patients. We used SAS 9.4 software for analyzing the data.
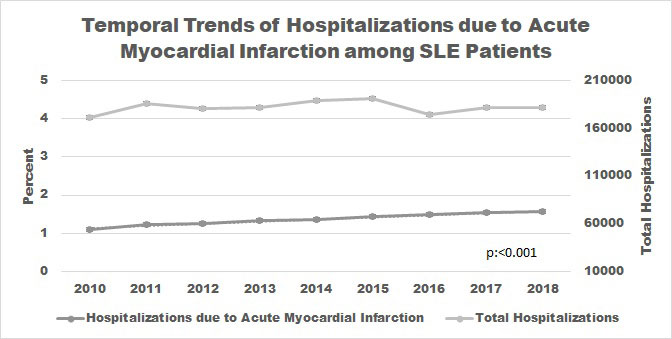
Results: Out of a total of 1,636,848 hospitalizations among SLE patients, 22,424 (1.4%) were due to primary diagnosis of AMI. Temporal trend of hospitalization due to AMI among SLE patients increased from 1,864 (1.1%) in 2010 to 2,835 (1.6%) in 2018 (p:< 0.001) with annual increase of 4% (OR 1.04; 95%CI 1.02-1.06; p< 0.0001). Even after adjusting with changes in demographics and comorbidities, we observed a similar trend. In multivariable regression analysis, we found that increasing age (OR 1.05; 95%CI 1.03-1.06; p< 0.0001), male gender (OR 1.35; 95%CI 1.34-1.38; p< 0.001), antiphospholipid antibodies (OR 1.17; 95%CI 1.01-1.37; p:0.045), smoking (OR 2.01; 95%CI 1.87-2.15; p< 0.0001) as well as comorbidities such as hypertension (OR 1.19; 95%CI 1.11-1.28; p< 0.0001), diabetes mellitus, chronic renal failure and obesity were associated with increased odds of hospitalization due to AMI among SLE patients. Overall, in-hospital mortality was higher during hospitalization due to AMI (4.6% vs 1.7%; p< 0.001) and the trend remained stable during the study period. Hospitalization due to AMI demonstrated mean length of stay of 5-days.
Conclusion: We observed a statistically significant increase in the trend of hospitalizations due to AMI among SLE patients from year 2010 to 2018. We identified several risk predictors such as demographics and comorbidities associated with higher odds of hospitalization due to AMI among SLE patients. Further in-depth studies are warranted to understand the causality of increased risk and formulate preventive strategies in the long run that would help mitigate the risk of AMI in SLE patients.
To cite this abstract in AMA style:
Bazigh I, Khan U, Patel A, Singh A, Ghalib N, Farman G, Muddassir S, Zaidi F, Mughni S, Grunbaum A. Trends and Predictors of Hospitalizations Due to Acute Myocardial Infarction in Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/trends-and-predictors-of-hospitalizations-due-to-acute-myocardial-infarction-in-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-and-predictors-of-hospitalizations-due-to-acute-myocardial-infarction-in-systemic-lupus-erythematosus-patients/