Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: In recent years, the American College of Rheumatology has stewarded a number of rheumatology-specific quality measures for use in national pay-for-performance programs. While the introduction of specialty-specific measures affords rheumatologists’ an opportunity to submit quality measures more applicable to their field, the uptake of such measures is unknown. Using RISE registry data, we investigated how often rheumatology-specific quality measures were submitted to the Merit-based Incentive Payment System (MIPS) and evaluated whether the use of these measures varied by practice characteristics.
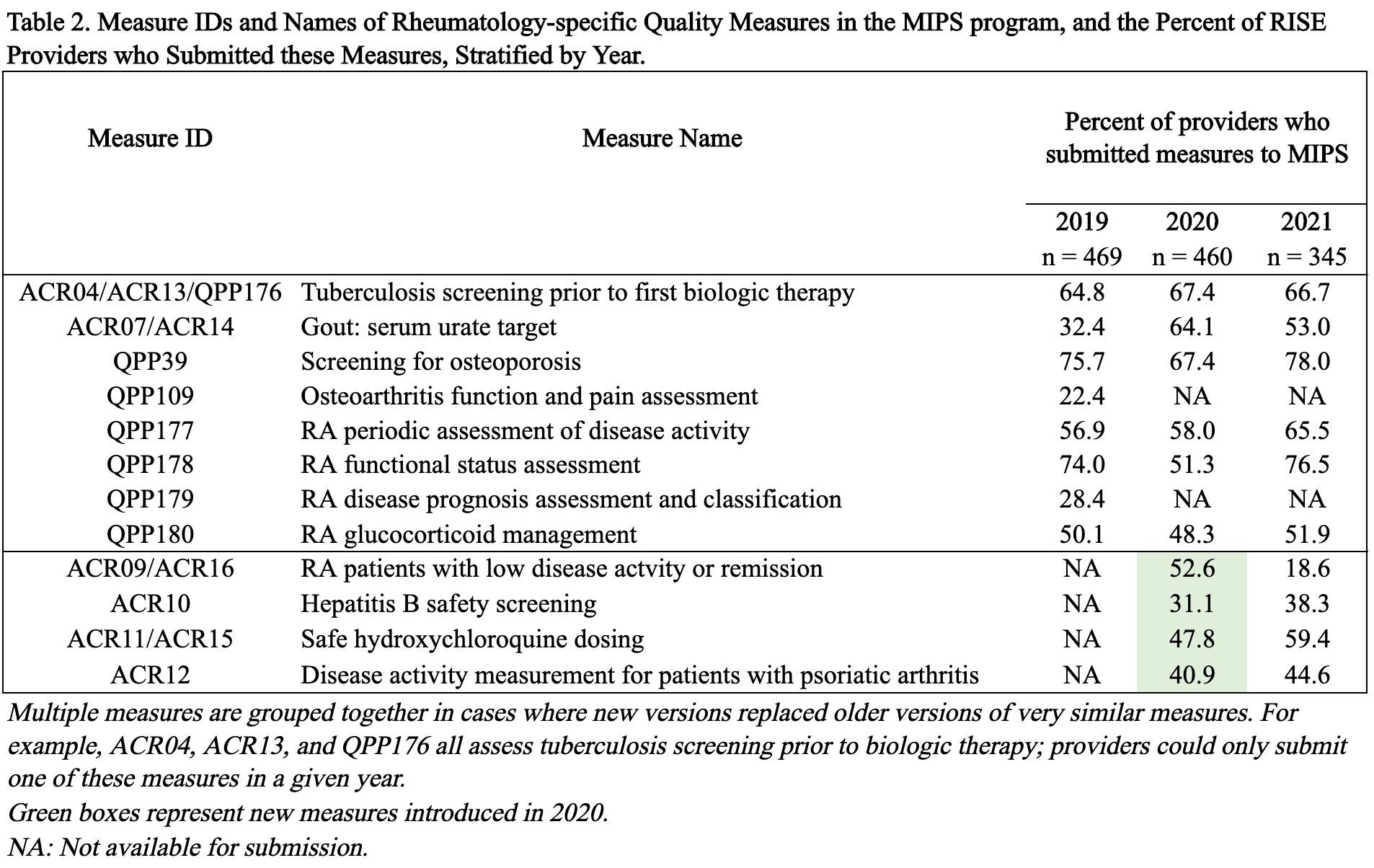
Methods: The RISE-registry’s MIPS dashboard contains information on group and individual MIPS submissions for participating practices and providers. Between 2019 and 2021, 12 quality measures were identified as rheumatology-specific since they aligned with care routinely provided by rheumatologists (Table 2). MIPS submissions were analyzed at the provider level: quality measures from individual submissions were prioritized over group submissions for the subset of providers that submitted as both an individual and as part of a group. Quality measures from group submissions were assigned to each participating clinician in the group for those without individual submissions. Using three years of MIPS submission data (2019 – 2021), we identified the most frequently submitted measures, determined the proportion of total rheumatology measures submitted and examined the uptake of new rheumatology-specific measures by practice type.
Results: We assessed 620 providers’ MIPS submissions from 156 practices. Most providers were from single-specialty practices (74%) and the South or Midwest regions (67%). Practices had a median of 6 clinicians and 6313 patients (Table 1). The number of rheumatology-specific measures available increased over time due to the debut of 4 new measures in 2020 including RA disease activity in low disease activity or remission (outcome measure); safe hydroxychloroquine dosing; Hepatitis B safety screening; and disease activity measurement for patients with psoriatic arthritis (Table 2). In parallel, the number of rheumatology-specific measures submitted to MIPS increased: overall, providers submitted a mean of 4 rheumatology measures in 2019, 5 in 2020, and 6 in 2021. In 2020, 75% of providers submitted at least 1 of the 4 new measures (range 31.1-52.6% for each measure); in 2021, this increased to 80% (range 18.6-59.4%). Single-specialty providers were most likely to adopt new rheumatology measures: 81% of single-specialty providers submitted at least 1 new measure compared to 55% of multi-specialty and 63% of solo practitioners.
Conclusion: RISE participating providers’ use of rheumatology-specific quality measures has been consistently high, and newly introduced measures have demonstrated substantial uptake. Future studies should investigate whether the submission of specialty-specific quality measures correlates with improved performance on quality measures as well as patient outcomes.
To cite this abstract in AMA style:
Kersey E, Li J, Izadi Z, Adler-Milstein J, Johansson T, Yazdany J, Schmajuk G. Uptake of Rheumatology-Specific Quality Measures Submitted to National Pay-for-Performance Programs: An Analysis of Participants in the RISE Registry [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/uptake-of-rheumatology-specific-quality-measures-submitted-to-national-pay-for-performance-programs-an-analysis-of-participants-in-the-rise-registry/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uptake-of-rheumatology-specific-quality-measures-submitted-to-national-pay-for-performance-programs-an-analysis-of-participants-in-the-rise-registry/