Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Pediatric uveitis is commonly associated with rheumatic disease and can lead to sight-threatening complications. Initial treatment are glucocorticoids and subsequently methotrexate (MTX) and TNF inhibitors for refractory uveitis. Autosomal dominant neovascular inflammatory vitreoretinopathy (ADNIV) is a rare autoimmune condition diagnosed in adults and characterized by intermediate uveitis, retinal degeneration and neovascularization. ADNIV is caused by a pathogenic variant in the Calpain-5 (CAPN5) gene. It is asymptomatic at presentation but inevitably leads to permanent blindness in later decades despite glucocorticoids, anti-VEGF and panretinal laser. Routine testing for CAPN5 and ophthalmic screening for uveitis is not regularly done in children. Our aim is to present the short-term outcomes of the first cohort of children diagnosed with ADNIV treated with methotrexate (MTX) and infliximab (IFX) to prevent poor vision outcomes.
Methods: Retrospective consecutive case series. Patients included were ≤21 years old at diagnosis, (+) CAPN5 gene mutation (c.731 T >C, p.Leu244Pro), and had ocular findings consistent with ADNIV. Treatment response was defined as a decrease in 1) vitreous cells on clinical examination, 2) retinal vascular leakage on ultra-widefield fluorescein angiography (UWFA), and/or 3) macular edema on optical coherence tomography (OCT).
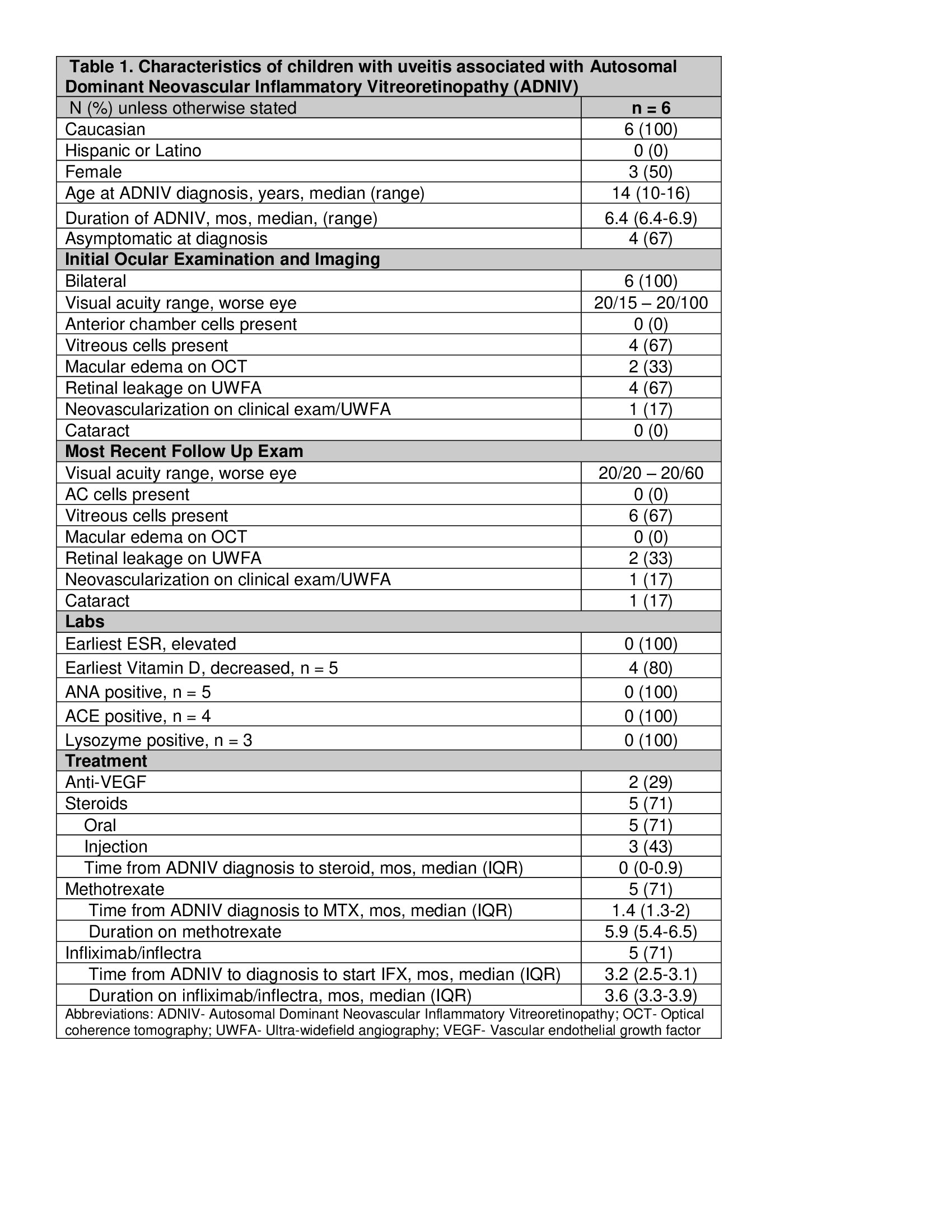
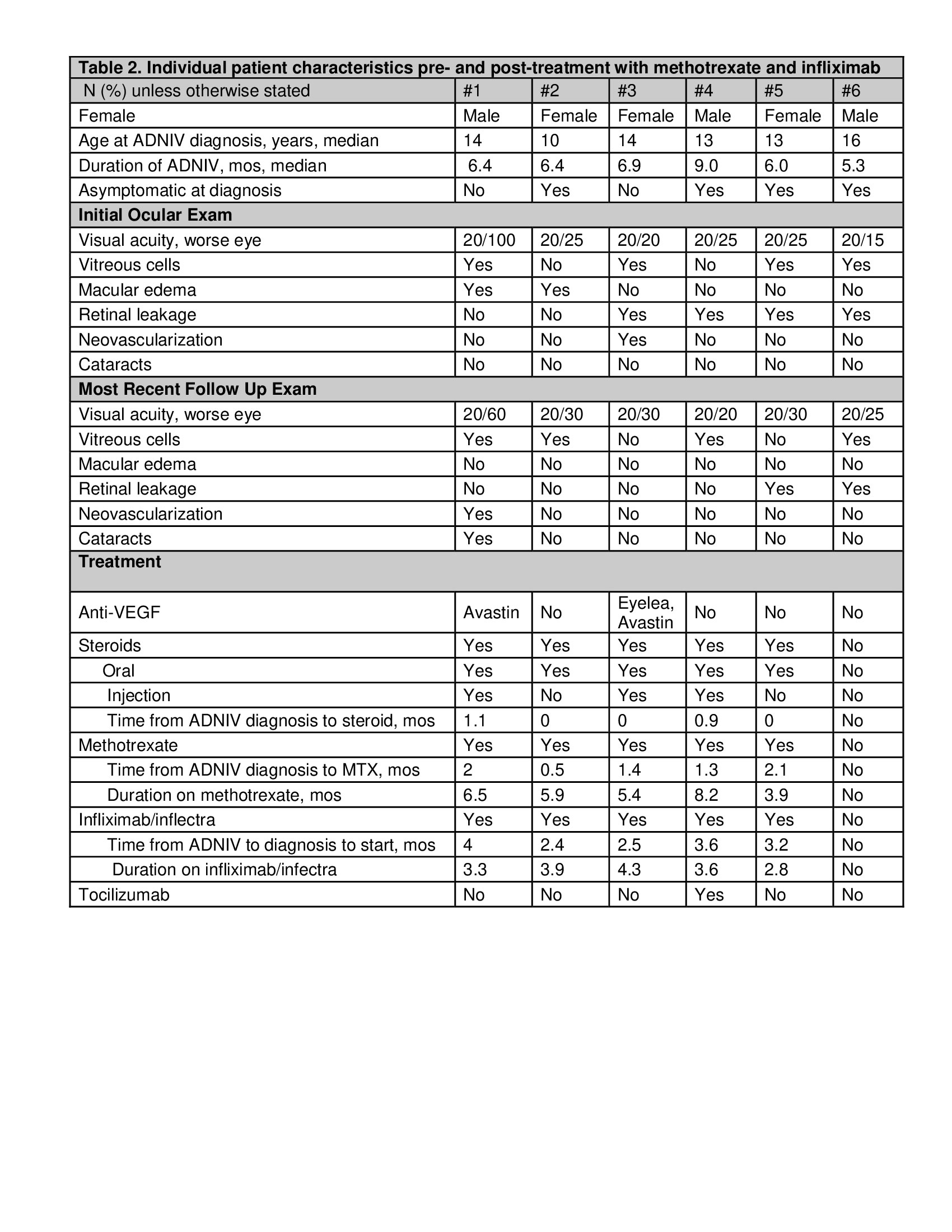
Results: Of 19 children with a family history of ADNIV, 9 were (+) for CAPN5. Six patients (12 eyes) were included in this study (Table 1). All were non-Hispanic whites, 50% were female, and diagnosed with ADNIV at a median age of 13 (range 10-16) years. The median disease duration was 6.4 (range 6.4-6.9) months. Four of 6 children were asymptomatic and diagnosed by clinical examination/imaging. At diagnosis, visual acuity in the worse eye was 20/80 or better, no anterior chamber cells, vitreous cells in 4 children, and cataract in 1. On UWFA, 4 had retinal vascular leakage and 1 had neovascularization. On OCT, 2 had macular edema. Earliest ESR was normal, ANA (n=5), ACE (n=4), and lysozyme (n=3) were negative. Vitamin D was decreased in 4/5. Five of the 6 children were initially treated with oral (n=4) or local/injected corticosteroids (n=3), and anti-VEGF therapy (n=2). Due to continued need for corticosteroids, 5 escalated to MTX (1 mg/kg [max 20 mg] weekly SQ) for a median duration of 5.9 (interquartile [IQR] 5.4-6.5) months. None responded to MTX, thus IFX or inflectra (10 mg/kg/dose every 4 weeks) was added for a mean duration of 3.6 (IQR 3.3-3.9) months. At last follow up, 4 improved on IFX, and 1 escalated to tocilizumab (Table 2).
Conclusion: We report on the first series of children with uveitis associated with ADNIV and treated with systemic immunosuppression. Delayed diagnosis and treatment leads to ischemia, neovascularization, and permanent vision loss. Early testing for CAPN5 gene in at risk children, and regular scheduled screening for uveitis and vasculitis will lead to prompt intervention. Similar to other non-infectious uveitis, timely treatment with MTX and IFX may alter the natural history of eventual blindness.
To cite this abstract in AMA style:
Angeles-Han S, Schulert G, Quinlan-Waters M, Duell A, Huggins J, Nguyen T, Sapp C, Sharma S, Srivastava S, Sood A. Outcomes of Children with Uveitis Associated with Autosomal Dominant Neovascular Inflammatory Vitreoretinopathy (ADNIV) Treated with Methotrexate and Infliximab [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-children-with-uveitis-associated-with-autosomal-dominant-neovascular-inflammatory-vitreoretinopathy-adniv-treated-with-methotrexate-and-infliximab/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-children-with-uveitis-associated-with-autosomal-dominant-neovascular-inflammatory-vitreoretinopathy-adniv-treated-with-methotrexate-and-infliximab/