Session Information
Date: Sunday, November 13, 2022
Title: Abstracts: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science
Session Type: Abstract Session
Session Time: 8:00AM-9:00AM
Background/Purpose: 20-25% of osteoporosis-related fractures occur in men and the mortality of osteoporotic fractures is higher in men [1]. Nevertheless, no uniform consensus exists for osteoporosis screening in men. The United States Preventive Services Task Force doesn’t recommend a specific age for osteoporosis screening in men [2]. Many other expert groups recommend osteoporosis screening for men 70 years and older [3-6].
Despite these recommendations, osteoporosis in this population remains underdiagnosed and undermanaged. We opted to study the rates of osteoporosis screening in elderly men in a large academic center, and further evaluate for potential racial disparities.
Methods: We conducted a retrospective cross-sectional study from a large urban academic medical center in Cleveland (the MetroHealth System). We evaluated the frequency of bone mineral density (BMD) scans performed in men and women aged 65 and above from 2010 through 2021. To further refine the data, we limited the data to the years of 2010, 2018 and 2021, and compared the data among three races (White, Black and Asian). Next, we further categorized the data in three age categories of 65 to 75, 75 to 85 and 85 and above. We also gathered data for hip fractures in the same cohort during the same years. Data from other minority groups and other fractures were excluded due to lack of sufficient data and potential inaccuracy.
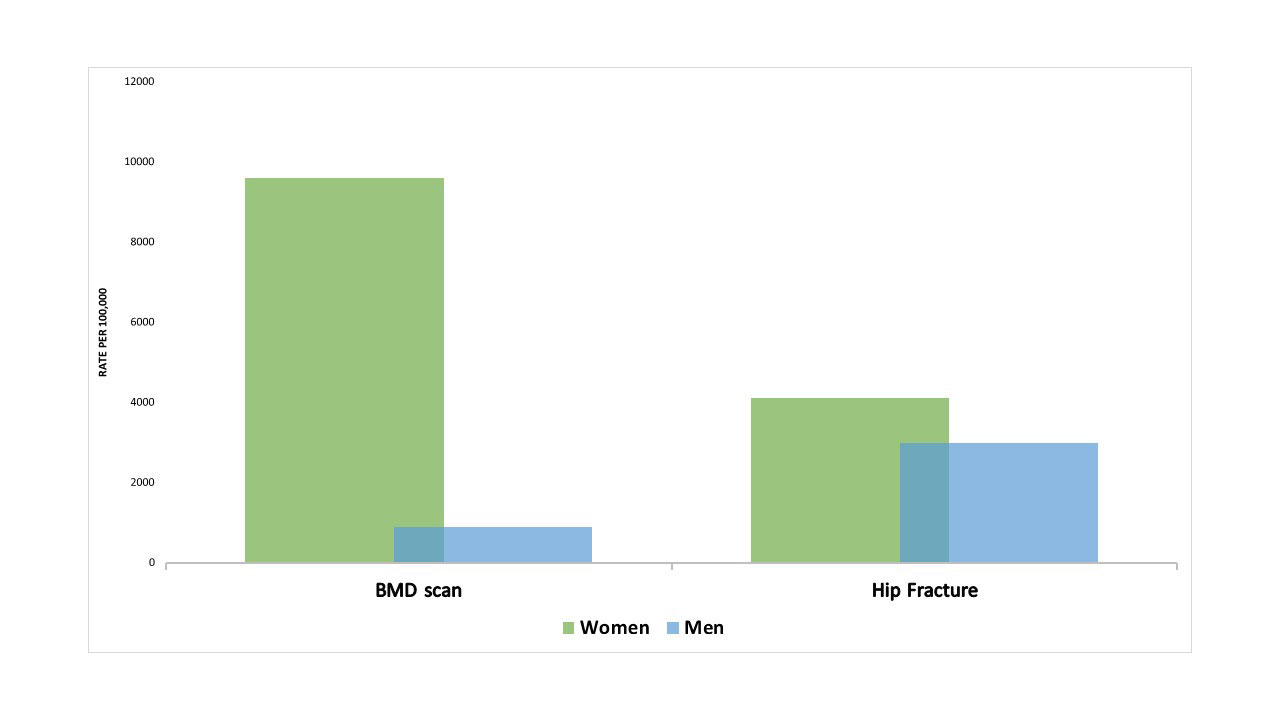
Results: The prevalence of BMD scan in women was 8.65%, while it was only 0.82% for men in our cohort. When looking at the data for 2010, 2018 and 2021, the same pattern was observed with BMD scan rates of below 1% in men and 7-10 % in women. A similar pattern of BMD scans was observed looking at three different age categories. The total rate of hip fracture was 4.1% in women, and 3% in men. Age-specific hip fracture rates in men and women were mostly similar.
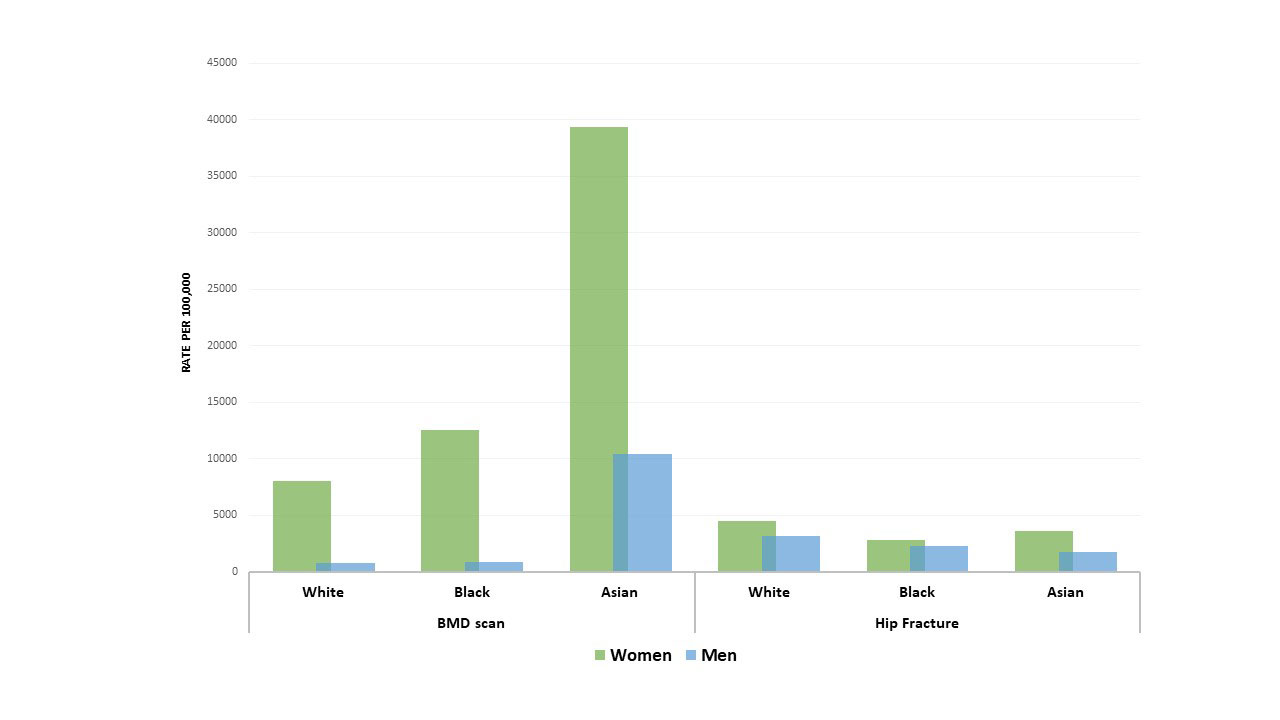
Asian women and men had higher rates of BMD scan compared to Blacks and Whites. However, no significant difference was observed in rates of BMD scan between Blacks and Whites. BMD scan rates declined in men from 2010 to 2018, and did not improve from 2018 to 2021. When analyzing data of hip fracture in the three races, no significant difference in rates of hip fracture was observed between Whites, Blacks and Asians.
Conclusion: Our study underscores the profoundly lower osteoporosis screening rates in men compared to women in a large academic center in Cleveland, United States. This is while hip fracture rate was only slightly lower in men than women.
Osteoporosis screening in minority groups of Blacks and Asians seems to be proportionate to the total patient population served by MetroHealth Medical Center, without significant difference between the three races. Also, no specific trend of hip fracture was observed between men in three races. On average the highest rates of BMD scans in men were observed in Asian men, while the overall lowest rate was seen in White men.
Our study is limited due to the retrospective nature and potential minor inaccuracy of data. However, the extremely low BMD scan rates despite relatively high rates of hip fracture in men are eye opening and should prompt further dedicated research in larger populations, hopefully leading to and unification of improved osteoporosis guidelines in elderly men.
To cite this abstract in AMA style:
Mollaeian A, Ballou S. Osteoporosis in Elderly Men; An Underestimated and Underdiagnosed Morbid Entity [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/osteoporosis-in-elderly-men-an-underestimated-and-underdiagnosed-morbid-entity/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoporosis-in-elderly-men-an-underestimated-and-underdiagnosed-morbid-entity/