Session Information
Date: Saturday, November 12, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Adults with ankylosing spondylitis (AS) are at a significantly increased risk of fracture relative to the general population. While some studies have evaluated the risk of fracture in AS, we do not have any U.S. population-level studies assessing all fracture types performed within the last three decades. We evaluated the incidence rate and factors associated with fractures among those with AS using linked data from the Rheumatology Informatics System for Effectiveness (RISE) registry and Medicare claims.
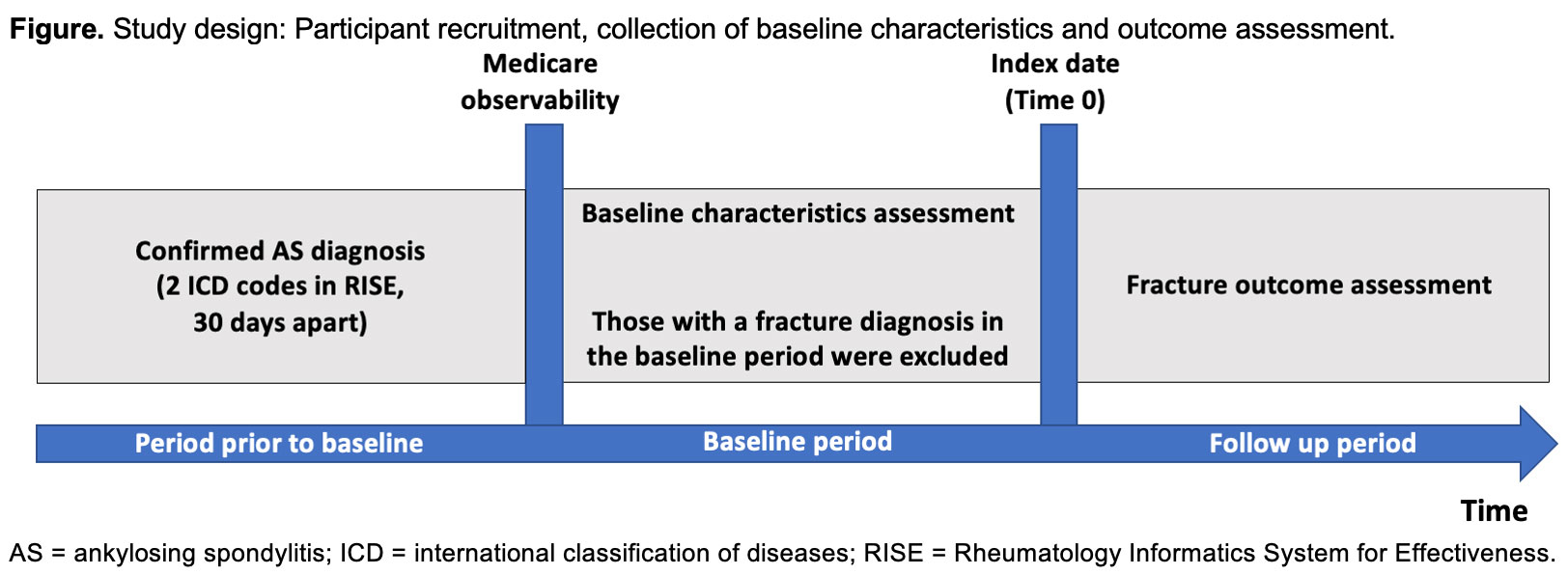
Methods: Data were derived from RISE, a large, national electronic health record-based registry, which was linked to Medicare claims from 2016-2018. Patients were required to have at least two visits for AS with a rheumatology provider, ≥ 30 days apart, prior to the baseline period of the study (Figure). Then, they were required to have at least one Medicare claim. Once this was confirmed, we collected one year of baseline characteristics from both RISE and Medicare claims. Patients with a fracture prior to the index date were excluded. Starting at the index date, patients were followed over time for fractures. Fractures were defined by ICD codes. We examined any fracture including those of the vertebra (cervical, thoracic, lumbar, sacral, and coccygeal), clavicle, ribs, sternum, humerus, ulna, distal radius, wrist, pelvis, hip, femur, knee, tibia, fibula, ankle, and foot. First, we calculated the incidence rate of fractures among individuals with AS. Second, logistic regression models were constructed to identify factors associated with fracture, including age, sex, race or ethnic group, body mass index (BMI), dual-eligibility for Medicare and Medicaid, area deprivation index, Charlson comorbidity index, smoking status, diagnosis of osteoporosis, and use of osteoporosis treatment, glucocorticoids, and opioids.
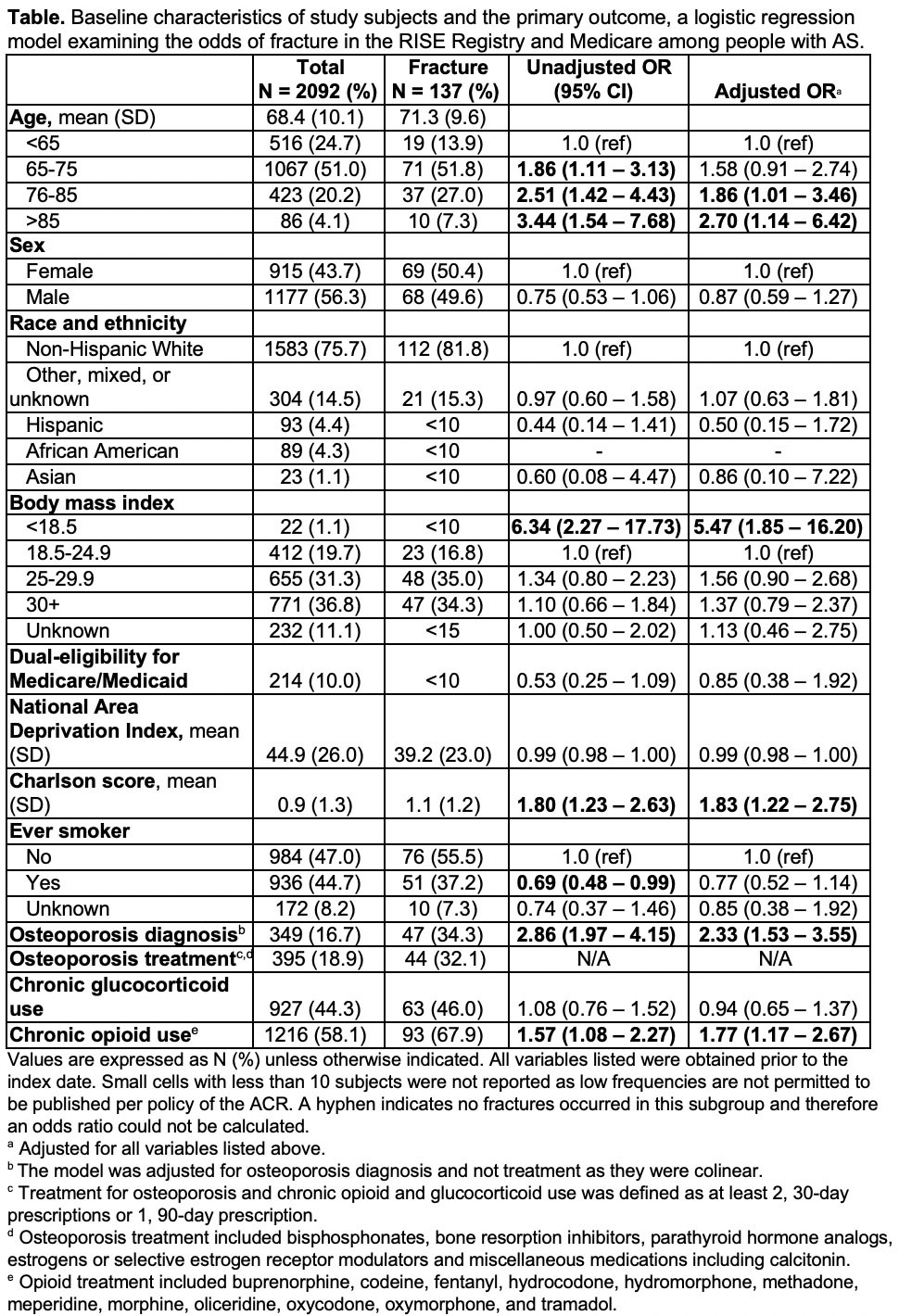
Results: We identified 2,092 adults with AS in RISE who were also observable in Medicare. The mean (SD) age was 68.4 years (10.1), 43.7% were female, and 75.7% were non-Hispanic White (Table). Ten percent had dual-eligibility for Medicare and Medicaid. Fractures occurred in 137 AS adults. The overall incidence rate of fractures among adults with AS was 37.01 (95% CI 31.31-43.76) per 1,000 person-years. Older age (OR 2.70, 95% CI 1.14 – 6.42), BMI < 18.5 (OR 5.47, 95% CI 1.85 – 16.20), higher Charlson comorbidity index (OR 1.83, 95% CI 1.22 – 2.75), osteoporosis diagnosis (OR 2.33, 95% CI 1.53 – 3.55), and chronic use of opioid drugs (OR 1.77, 95% CI 1.17 – 2.67) conferred increased odds of fracture.
Conclusion: In this large U.S. sample of older adults with AS, those who were older, had a low BMI, had multiple comorbidities including osteoporosis, and used opioids chronically had a higher odds of fracture. Men and women with AS were equally likely to have a fracture, unlike in the general population where women are known to be at higher risk. Because chronic opioid use was associated with fracture in AS, this high-risk population should be considered for interventions to mitigate risk.
Disclaimer: Data collection was supported by the ACR’s RISE Registry. The views expressed represent those of the authors, not necessarily those of ACR.
To cite this abstract in AMA style:
Stovall R, Kersey E, Li J, Baker R, Anastasiou C, Schmajuk G, Gensler L, Yazdany J. Incidence Rate and Factors Associated with Fractures Among Older Adults with Ankylosing Spondylitis in the United States [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/incidence-rate-and-factors-associated-with-fractures-among-older-adults-with-ankylosing-spondylitis-in-the-united-states/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-rate-and-factors-associated-with-fractures-among-older-adults-with-ankylosing-spondylitis-in-the-united-states/