Session Information
Date: Saturday, November 12, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with chronic back pain (CBP; back, buttock, or hip pain ≥ 3 months) where the underlying cause may be axSpA are usually first seen in non-rheumatology settings such as chiropractic clinics. These settings lack consistency in referral to rheumatologists, which may lead to delays in diagnosis. In a previous study1, where chiropractors referred patients with CBP as the primary complaint, originating from sacroiliac (SI) joints according to the chiropractor, plus at least one SpA feature to a rheumatologist, the prevalence of axSpA was found to be 6.8%. The objective of this study was to assess the prevalence of undiagnosed axSpA in patients attending chiropractic clinics with a primary or secondary complaint of CBP, and referred with the Assessment of Spondyloarthritis International Society (ASAS) referral strategy.
Methods: Eligible patients were adults attending one of four chiropractic clinics in the United States between November 2020 and November 2021 with CBP starting before age of 45, without prior diagnosis of SpA. Patients were referred to a rheumatologist for diagnostic assessment via phone consultation if they had ≥1 of the following features: inflammatory back pain (IBP), a family history of SpA, inflammatory bowel disease (IBD), psoriasis, good response to NSAIDs, history of heel pain, uveitis, or peripheral arthritis. The subsequent rheumatology assessment included medical history (telephone interview), laboratory tests (CRP, HLA-B27), x-ray and MRI of SI joints. An academic rheumatologist made the diagnosis of axSpA, peripheral SpA, or absence of SpA.
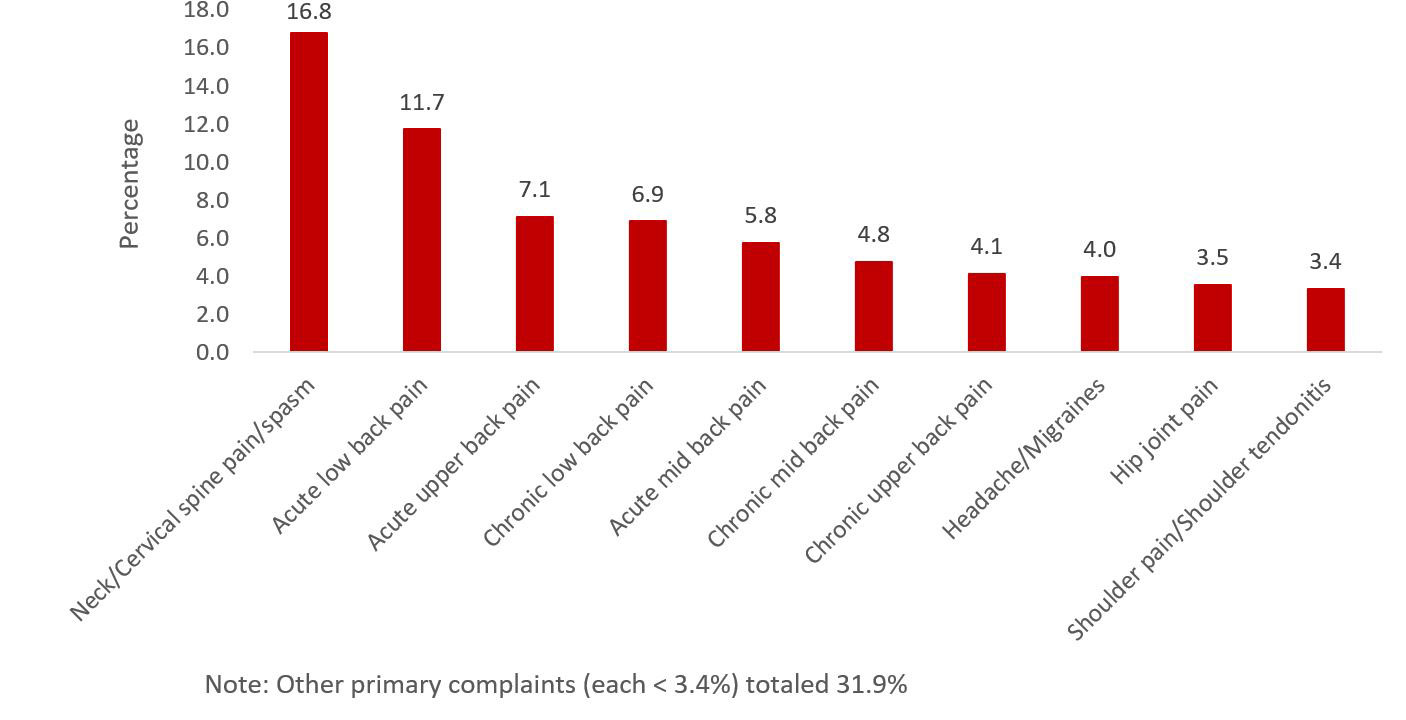
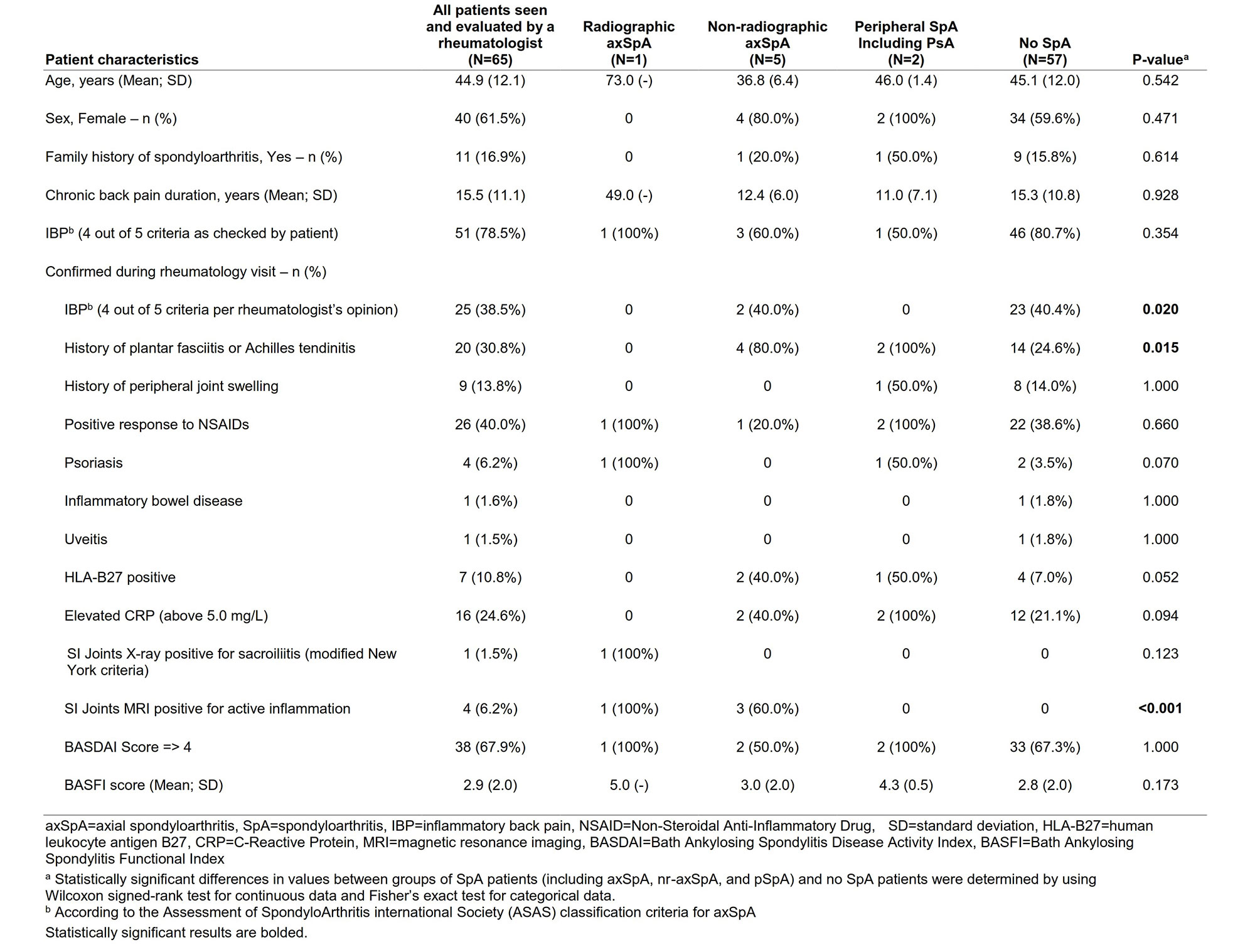
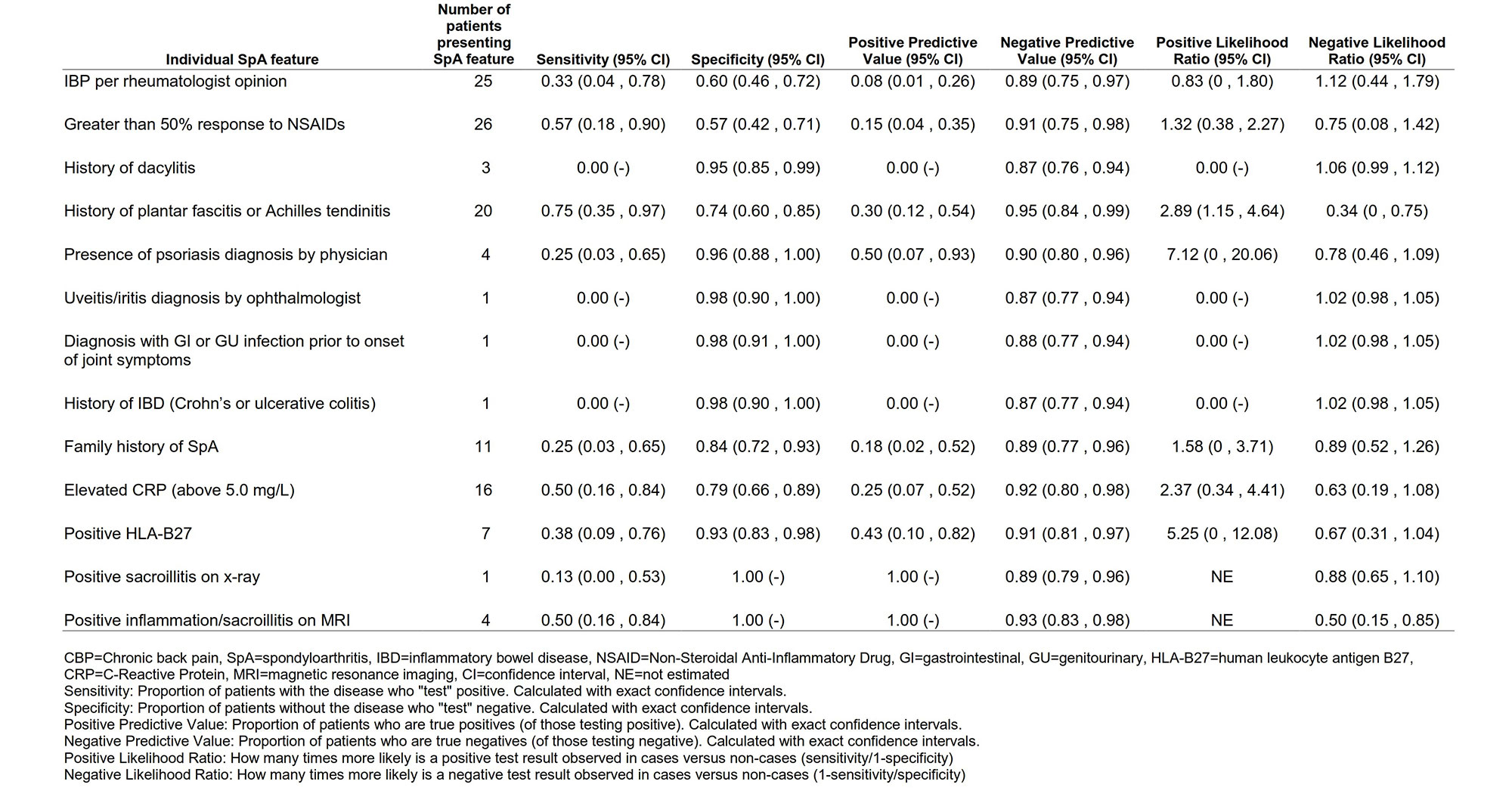
Results: A total of 3,103 visits were recorded at 4 chiropractic clinics during the study period. Top 10 primary complaints at chiropractic visits are presented in Figure 1. In total, 115 patients were referred, and of the 74 who were eligible and provided consent, 59 (79.7%) reported to have IBP. In total, 65 patients were fully assessed by a rheumatologist, of which 8 (12.3%) had SpA. Five (7.7%) were diagnosed as non-radiographic axSpA (nr-axSpA, fulfilled ASAS classification criteria), 1 (1.5%) radiographic axSpA (fulfilled modified New York criteria), 1 (1.5%) Psoriatic Arthritis without imaging evidence of axial involvement (fulfilled Classification Criteria for Psoriatic Arthritis), and 1 (1.5%) had undifferentiated peripheral SpA (fulfilled ASAS Classification Criteria). Patient characteristics are presented in Table 1. Out of the SpA features, objective parameters such as imaging, presence of psoriasis and positive HLA-B27 had the highest positive likelihood ratio (Table 2).
Conclusion: Twelve percent of patients with CBP referred from chiropractic clinics with the ASAS strategy had undiagnosed SpA, with nr-axSpA being the most common. Our sample indicates that objective features of inflammation have the highest positive likelihood ratio in making the diagnosis of SpA.
1Kiwalkar et al. Chiropractic Axial Spondyloarthritis Study (ORCAS): Interim Results [Abstract] SPARTAN Annual Meeting 2020
To cite this abstract in AMA style:
Deodhar A, Kiwalkar S, Phung Nguyen K, Quinn R, Perham D, Malatestinic W, Bolce R, Hunter T, Khurana P, Bhalerao S. Prevalence of Axial Spondyloarthritis (axSpA) in Patients Treated for Chronic Back Pain in Chiropractic Clinics [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-axial-spondyloarthritis-axspa-in-patients-treated-for-chronic-back-pain-in-chiropractic-clinics/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-axial-spondyloarthritis-axspa-in-patients-treated-for-chronic-back-pain-in-chiropractic-clinics/