Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Interstitial lung disease (ILD) is one of the main comorbidities of patients with RA contributing to an increased mortality risk [1]. The pathogenesis of RA-ILD remains poorly defined, constituting its early diagnosis a challenge for clinicians [1]. The endothelium plays a pivotal role in inflammatory diseases and in the pulmonary vascular regulation contributing to the development of vascular dysfunction and the subsequent onset and progression of ILD [2,3]. Accordingly, the objective of this work was to elucidate the role of monocyte chemoattractant protein-1 (MCP-1), vascular cell adhesion protein 1 (VCAM-1) and asymmetric dimethylarginine (ADMA), key molecules in endothelial dysfunction, in the pathological processes of both underlying vascular damage and pulmonary fibrosis in RA-ILD.
Methods: Peripheral venous blood was collected from 21 patients with RA-ILD+ and individuals from 3 comparative groups: 25 patients with RA-ILD–, 21 patients with idiopathic pulmonary fibrosis (IPF) and 21 healthy controls (HC). All the individuals were recruited from the Rheumatology and Pneumology departments of Hospital Universitario Marqués de Valdecilla, Santander, Spain. Serum levels of MCP-1, VCAM-1 and ADMA were measured by enzyme-linked immunosorbent assay.
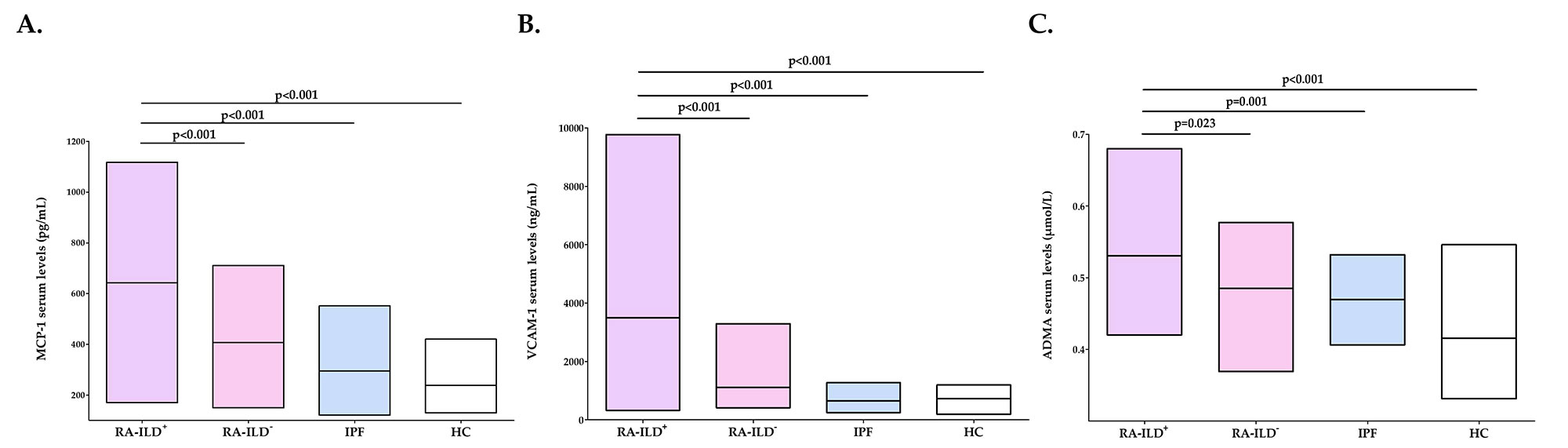
Results: Patients with RA-ILD+ exhibited significantly higher serum levels of MCP-1, VCAM-1 and ADMA in relation to HC (p< 0.001 in all cases, Figure 1A-C). Likewise, increased levels of MCP-1, VCAM-1 and ADMA were found in patients with RA-ILD+ compared to those with RA-ILD– (p< 0.001, p< 0.001 and p=0.023 respectively, Figure 1A-C). It was also the case when patients with RA-ILD+ were compared with patients with IPF (p< 0.001, p< 0.001 and p=0.001, respectively, Figure 1A-C).
Conclusion: Our study supports a role of MCP-1, VCAM-1 and ADMA in the underlying vasculopathy in RA-ILD+. Interestingly, an increase of serum levels of MCP-1, VCAM-1 and ADMA may help to identify the presence of ILD in patients with RA and to discriminate RA-ILD+ patients from those with IPF.
References: [1] J Clin Med 2019;8(12):2038; [2] Stem Cell Rev Rep 2018;14(2):223-235; [3] Atherosclerosis 2012;224(2):309-317.Personal funds, VP-C and SR-M: RD16/0012/0009(ISCIII-ERDF); FG: RICORS Program (RD21/0002/0025) (ISCIII-EU); RL-M: CP16/00033 (ISCIII-ESF).
To cite this abstract in AMA style:
Pulito-Cueto V, Remuzgo-Martinez S, Genre F, Atienza-Mateo B, Mora-Cuesta V, Iturbe-Fernández D, Lera-Gómez L, Prieto-Peña D, Portilla V, Blanco R, Corrales A, Gualillo O, Cifrián J, Lopez Mejias R, González-Gay M. Monocyte Chemoattractant Protein-1, Vascular Cell Adhesion Protein-1 and Asymmetric Dimethylarginine as Potential Biomarkers of Interstitial Lung Disease Associated with RA [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/monocyte-chemoattractant-protein-1-vascular-cell-adhesion-protein-1-and-asymmetric-dimethylarginine-as-potential-biomarkers-of-interstitial-lung-disease-associated-with-ra/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/monocyte-chemoattractant-protein-1-vascular-cell-adhesion-protein-1-and-asymmetric-dimethylarginine-as-potential-biomarkers-of-interstitial-lung-disease-associated-with-ra/