Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Social determinants of health (SDoH), “the conditions in which people are born, grow, work, live, and age” (World Health Organization, 2022), directly influence health inequities. In our multihospital system, SDoH are not systematically assessed as part of routine rheumatic disease care. We studied patients with rheumatic conditions enrolled in an integrated care management program (iCMP), which provides care coordination for medically and/or psychosocially complex patients. We aimed to understand the documentation of SDoH-related needs during iCMP enrollment in electronic medical record (EMR) notes and whether the prevalence differed by rheumatic condition.
Methods: Among 20,395 adults (≥18 years) with ≥1 ICD-9/10 code for a systemic rheumatic condition, crystalline arthritis or osteoarthritis enrolled in iCMP between 1/1/12-10/18/21, we randomly selected 401 individuals. We excluded 18 individuals with insufficient EMR data. We reviewed the literature (SU, MC) to develop a set of SDoH-related terms related to financial needs, food insecurity, housing instability, transportation, and medication access and the most frequently used phrases were used to develop the standard operating procedure for the chart reviews. Charts were manually reviewed (SU, MC, CF) and SDoH phrases were extracted from EMR notes written by physicians, nurses, care coordinators, social workers, and nutritionists during iCMP enrollment. Patients were classified by whether they had any indication of documented SDoH-related needs. We used multivariable logistic regression to estimate the odds of having ≥1 SDoH need by demographic factors and rheumatic condition.
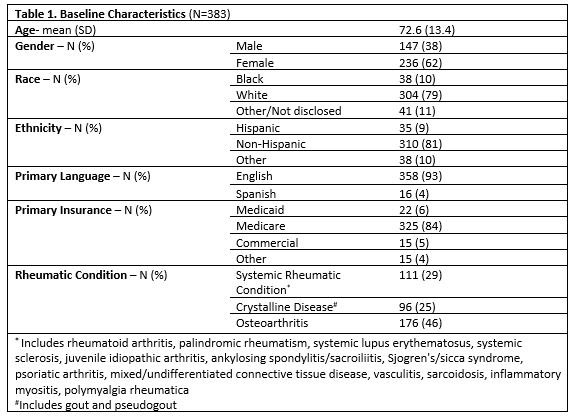
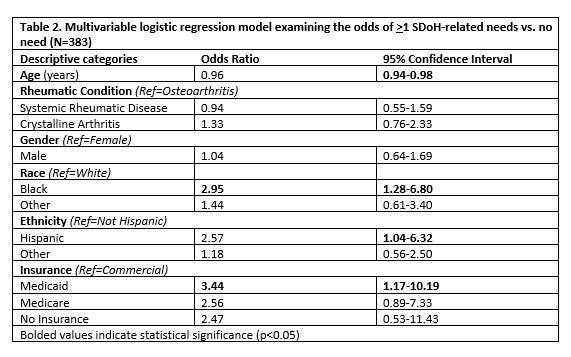
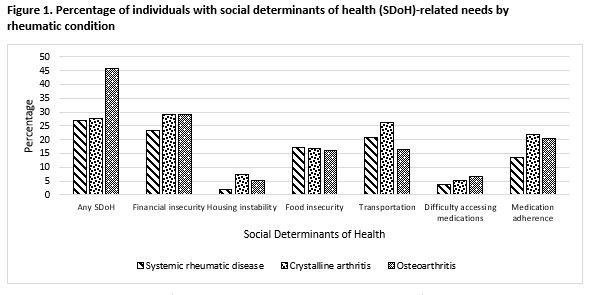
Results: Among 383 patients, the mean (SD) age was 72.2 (13.4) years, 61% were female, 79% were White, 10% were Black, and 80% were non-Hispanic (Table 1). The mean (SD) period of iCMP enrollment was 3.3 (2.4) years. There were 111 patients (29%) with a systemic rheumatic disease, 96 (25%) with crystalline arthritis, and 176 (46%) with osteoarthritis without systemic or crystalline disease. Of the 383 charts reviewed, 45% contained documentation of ≥1 SDoH need. Overall, 105 individuals (27%) had evidence of financial needs, 77 (20%) transportation needs, 63 (16%) food insecurity, 18 (5%) housing instability, and 21 (5%) medication access challenges, with variation by rheumatic condition (Figure 1). In the multivariable model, the odds of having ≥1 SDoH need was 2.85 times higher (95% CI 1.28-6.80) for Black vs. White individuals and 3.44 times higher (95% CI 1.17-10.19) for Medicaid vs. Commercial insurance beneficiaries (Table 2).
Conclusion: Nearly half of this population of complex care patients with rheumatic conditions had SDoH needs documented in EMR notes with the highest overall percentage among individuals with osteoarthritis. Higher burden was noted among Black individuals and Medicaid beneficiaries, however SDoH documentation was infrequently structured or standardized in notes, and differences may, in part, reflect ascertainment bias. Further efforts are needed to incorporate SDoH screening into routine rheumatology care, enabling integration of SDoH factors into both clinical care and research.
To cite this abstract in AMA style:
Ulysse S, Chandler M, Santacroce L, Cai T, Liao K, Feldman C. Documentation of Social Determinants of Health Among Individuals with Systemic Rheumatic and Musculoskeletal Diseases [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/documentation-of-social-determinants-of-health-among-individuals-with-systemic-rheumatic-and-musculoskeletal-diseases/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/documentation-of-social-determinants-of-health-among-individuals-with-systemic-rheumatic-and-musculoskeletal-diseases/