Session Information
Date: Saturday, November 12, 2022
Title: Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Diagnostic uncertainty is a common problem faced by rheumatologists. Even among patients under the care of a rheumatologist, patients may have one rheumatic illness that evolves into another, or two rheumatic conditions that co-exist. RA and SLE are the most common autoimmune conditions seen in rheumatology clinics, and patients with an overlap of signs and symptoms from each of these conditions are not unusual. We used the American College of Rheumatology’s RISE registry to identify different diagnostic code trajectories using RA and SLE as example conditions.
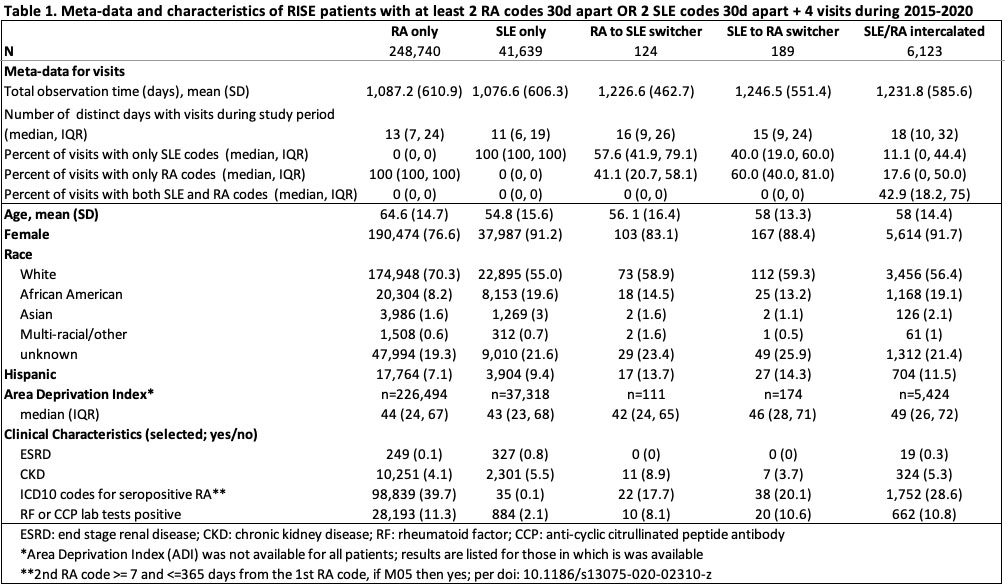
Methods: We used ICD codes from patients with data in the RISE registry. We included patients with at least 2 codes, 30 days apart for either RA or SLE and a minimum of 4 visits between Jan 2015 and June 2020. ICD codes from each visit were extracted. Patients were classified into mutually exclusive groups: visits with RA codes only; SLE codes only; switchers (only RA codes followed by only SLE codes or vice versa); or intercalated diagnoses (RA and SLE codes alternating over time or both occurring on the same day). We described each cohort according to “meta-data” regarding the number and proportion of visits with RA and/or SLE codes, as well as selected patient clinical characteristics.
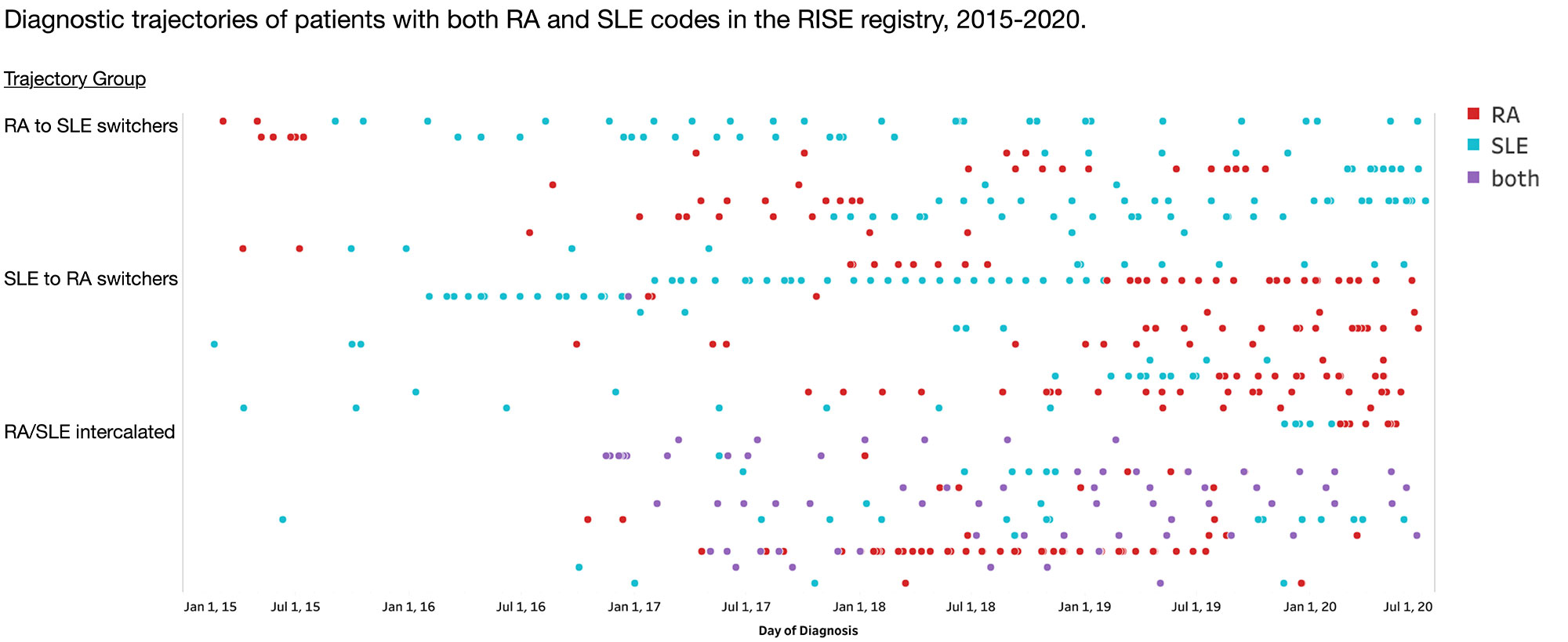
Results: 296,815 from 232 practices were included. We found 248,740 patients with visits with RA codes only; 41,639 with SLE only; and 6,436 patients with at least 2 codes, 30 days apart for both RA and SLE. Among these 6,436, 2% were RA to SLE switchers; 3% were SLE to RA switchers; 95% had RA and SLE diagnoses intercalated over time (Figure). Observation time (time from first visit to last visit during study period) was 20% higher for patients with codes for both RA and SLE compared to those with only RA or only SLE, as was the number of distinct days with visits. The percentage of visits with RA, SLE, or both codes varied by group – among switchers, the final diagnosis was also the diagnosis accounting for a greater proportion of the total codes (e.g. for RA to SLE switchers, the median for percent of visits with SLE codes only was 58%). For the intercalated group, a median of 43% of visits had both RA and SLE coded on the same day. Selected clinical characteristics of patients in each group are also shown in Table 1: patients in any category with at least 2 SLE codes tended to be younger and were more often non-white compared to patients with only codes for RA. Many patients with both RA and SLE codes were RF or CCP antibody positive, which distinguished them from patients with SLE only (47% vs. 2%, p < 0.001).
Conclusion: In this large population-based sample of patients, most patients had a stable diagnosis of either RA or SLE. A small minority of patients switched from one diagnosis to another – more often from SLE to RA than vice versa. Our findings support data from smaller studies suggesting that around 10% of patients with SLE codes will have a RA/SLE overlap syndrome. Future work will include detailed chart reviews to confirm these patterns and to define the minimum observation time and number of codes required to achieve diagnostic certainty in patients with these conditions.
To cite this abstract in AMA style:
Ituarte t, Li J, Kay J, Izadi Z, Yazdany J, Schmajuk G. Rheumatic Diagnostic Code Trajectories for Patients with RA and SLE in a U.S. Rheumatology Registry [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/rheumatic-diagnostic-code-trajectories-for-patients-with-ra-and-sle-in-a-u-s-rheumatology-registry/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatic-diagnostic-code-trajectories-for-patients-with-ra-and-sle-in-a-u-s-rheumatology-registry/