Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at increased risk of cognitive impairment compared to the general population. This association might be due to chronic systemic inflammation and the associated cardiovascular risk factors (Sood A and Raji MA, 2021). Studies on RA and neuroimaging biomarkers associated with cognitive impairment are limited. The purpose of the study was to examine the associations between RA and dementia/vascular neuroimaging biomarkers in older adults.
Methods: The study included 34 RA cases and 101 participants without RA (≥50 years old) of a prospective study of cognitive aging in community-dwelling older adults, matched 1:3 for age, sex, education, cognitive status at baseline, and the availability of at least one MRI. All RA cases satisfied the 1987 ACR classification criteria. The outcomes of interest were the following neuroimaging biomarkers: global beta-amyloid (Aβ) using PiB-PET; neurodegeneration [glucose brain hypometabolism via FDG-PET, hippocampal volume and cortical thickness via structural MRI], and cerebrovascular pathology via FLAIR-MRI [white matter hyperintensity burden (WMH), subcortical, and cortical infarctions]. All participants had MRI; 47 (12 RA /35 non-RA) had Aβ PET, 45 (10 RA / 35 non-RA) had FDG PET, 55 (17 RA / 38 non-RA) were assessed for infarctions and 49 (14 RA / 35 non-RA) for WMH%TIV. We used Kruskal-Wallis rank-sum and Fisher’s exact tests to compare the neuroimaging measures between the groups.
Results: Participants with vs. without RA did not differ in age, sex, years of education, Apolipoprotein E ε4 carrier status, or major comorbidities. No significant difference was observed between RA cases and non-cases in Aβ burden, and neurodegeneration measures. Although the sample size was small, we observed that RA participants (vs. without RA) had greater mean WMH volume relative to the total intracranial volume (TIV) (mean (SD) % : 1.12 (0.57) % vs 0.76 (0.69) % of TIV, p=0.01), were more likely to have cortical infarctions (4 vs. 1, p = 0.03), and had a higher mean (SD) number of cortical infarctions (0.24 (0.44) vs. 0.05 (0.32) (p=0.02) (Table 1). These associations persisted when the comparisons were limited to cognitively unimpaired individuals.
Conclusion: Patients with RA had more abnormalities in cerebrovascular imaging biomarker measures compared to individuals without RA, despite similar sociodemographics, Apolipoprotein E ε4 carrier status, markers of neurodegeneration, and similar proportion of cognitively impaired patients between the groups. Studies are ongoing to examine these associations further and understand their potential value for prognostication and prevention of cognitive decline and dementia in RA patients.
Reference: Sood A, Raji MA. Cognitive impairment in elderly patients with rheumatic disease and the effect of disease-modifying anti-rheumatic drugs. Clin Rheumatol. 2021 Apr;40(4):1221-1231
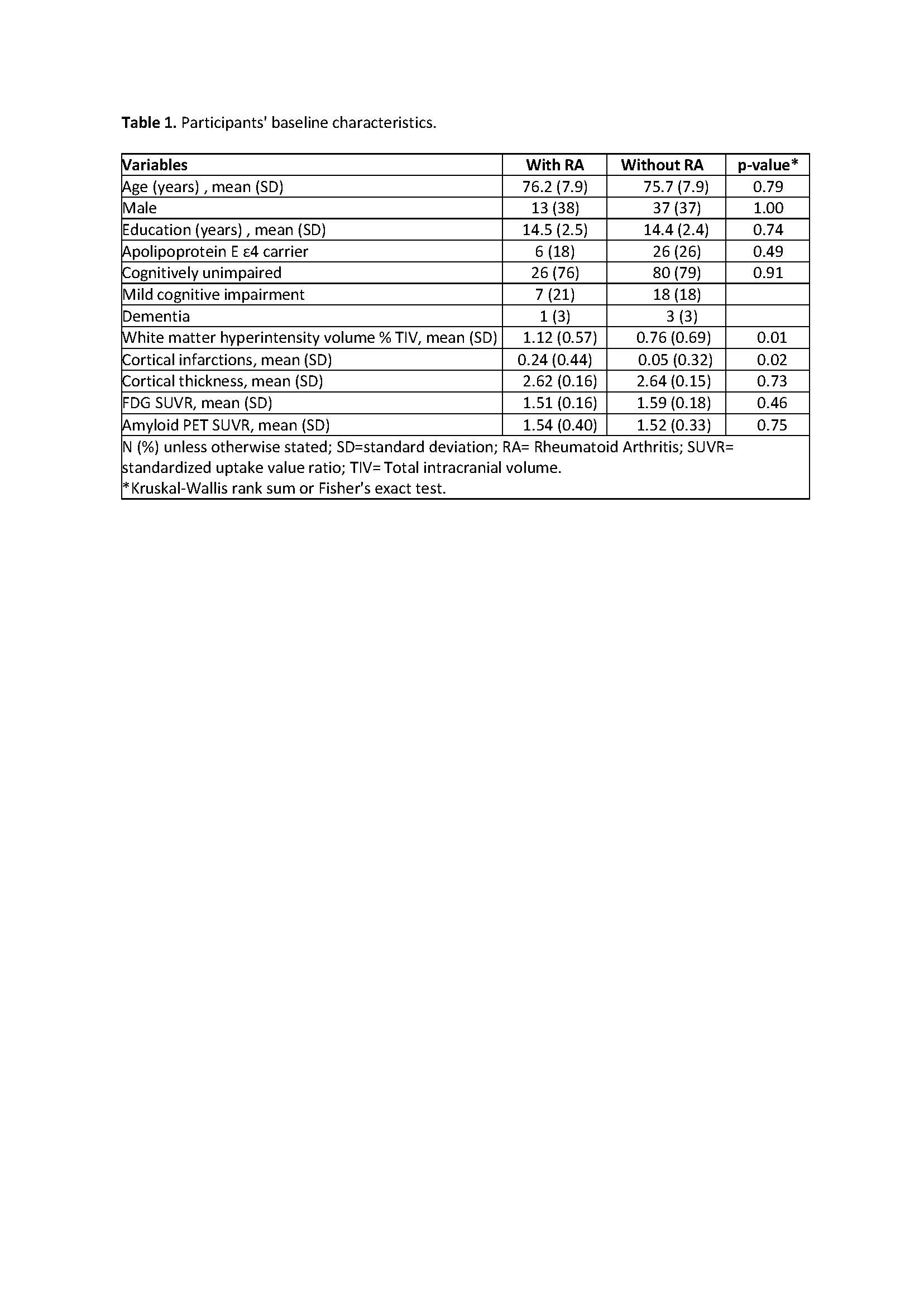 Table 1. Participants’ baseline characteristics.
Table 1. Participants’ baseline characteristics.
To cite this abstract in AMA style:
Vassilaki M, Crowson C, Davis J, Duong S, Nguyen A, Jones D, Mielke M, Prashanthi V, Myasoedova E. Abnormal Cerebrovascular Biomarkers in Patients with Rheumatoid Arthritis: Results from a Prospective Study of Cognitive Aging [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/abnormal-cerebrovascular-biomarkers-in-patients-with-rheumatoid-arthritis-results-from-a-prospective-study-of-cognitive-aging/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/abnormal-cerebrovascular-biomarkers-in-patients-with-rheumatoid-arthritis-results-from-a-prospective-study-of-cognitive-aging/
