Session Information
Date: Monday, November 8, 2021
Title: Plenary III (1424–1429)
Session Type: Plenary Session
Session Time: 11:30AM-11:45AM
Background/Purpose: A third of RA patients use long-term glucocorticoids (GCs) despite a known dose-dependent association with major adverse cardiovascular (CV) events (MACE). Prior work suggests long-term GC use is common among RA patients with MACE risk factors. We know little about the incremental effect of ongoing GC use on MACE risk in RA patients.
Methods: In this retrospective cohort study, we used national VA administrative data to identify RA patients with ≥1 rheumatology visit during 2013-2018. We defined the index date as the first rheumatology visit in this period after meeting RA diagnostic criteria. We excluded patients < 40 or >90 years and those with other rheumatologic disorders, prior MACE, or congestive heart failure during a lookback period of up to 5 years (Fig. 1). We used pharmacy dispensing data to calculate days’ supply of GC (exposure), and claims to identify incident MACE (outcome). We defined MACE as any of acute myocardial infarction, stroke, transient ischemic attack, cardiac arrest, or coronary revascularization. We used multilevel logistic regression to evaluate the association between days’ supply of GC dispensed in a 6-month period, and the lagged outcome of incident MACE in the following 6-month period. Patients were censored after their first MACE event. We adjusted for baseline covariates including demographics, healthcare utilization, and long-term GC use ( >90 days), and time-varying covariates including methotrexate and biologic use. We also adjusted for baseline MACE risk using the Veteran’s Affairs Risk Score for CV Disease (VARS-CV), developed to recalibrate the ACC/AHA risk calculator for the Veteran population. The algorithm uses medical and pharmacy claims, vital signs, and lab results to calculate a continuous risk prediction estimate, but can also categorize 5-year MACE risk as low (< 3%), medium (3-9%) or high ( >9%) using cut points from the ACC/AHA algorithm.
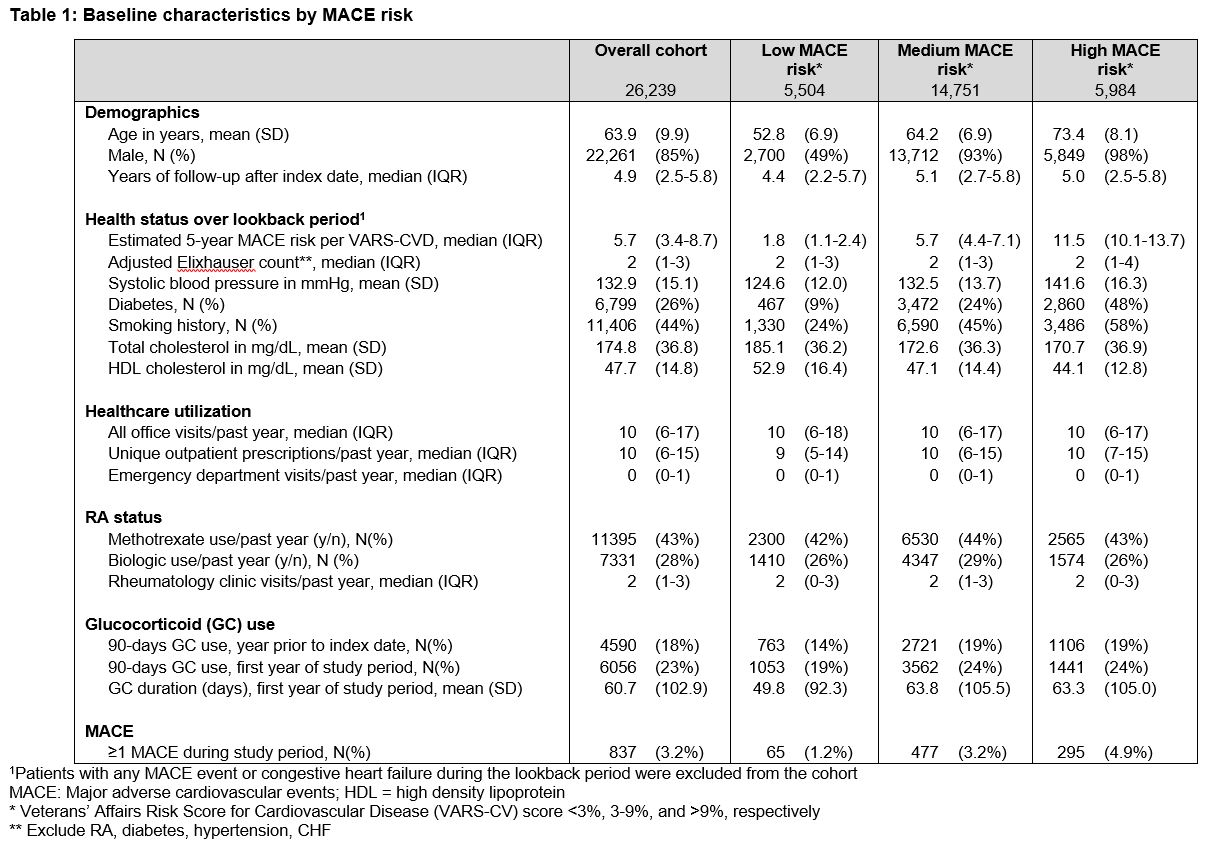
Results: Among 26,239 patients, median 5-year MACE risk by VARS-CV at baseline was 5.7% (IQR 3.4-8.7); 5,984 patients (23%) had high MACE risk (Table 1). Twenty-three percent of patients overall, and 24% with high MACE risk, received ≥90 days of GCs during Year 1 of followup. Incident MACE occurred in 3.2% of patients overall, and 4.9% of patients with high MACE risk. Median (IQR) time to incident MACE was 25 (12-44) months. After adjustment for the covariates above, ach additional 30 days of GC use in a 6-month period was associated with a 1.14 (95% CI 1.10-1.19) increase in odds of MACE in the following 6-month period (Table 2).
Conclusion: In this national RA cohort, 30 days of GC use in a 6-month period was associated with a 14% increase in odds of MACE over the subsequent 6 months. This association was independent of baseline CV, risk, prior long-term GC exposure, and claims-based markers of RA severity such as biologic use. Future work should be directed towards evaluating the effect of persistent GC use on rates of additional MACE events among those who have experienced prior MACE, and examining how baseline MACE risk impacts the relative effect of GC use on incident MACE.
To cite this abstract in AMA style:
Wallace B, Gao Y, Roul P, Cohen-Mekelberg S, England B, Mikuls T, Clauw D, Wiitala W, Hayward R, Sussman J, Waljee A. Association Between Ongoing Glucocorticoid Use and Major Adverse Cardiovascular Events Among Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-between-ongoing-glucocorticoid-use-and-major-adverse-cardiovascular-events-among-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-ongoing-glucocorticoid-use-and-major-adverse-cardiovascular-events-among-veterans-with-rheumatoid-arthritis/