Session Information
Date: Sunday, November 7, 2021
Title: Pediatric Rheumatology – Clinical Poster II: SLE, JDM, & Juvenile Scleroderma (0764–0785)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Lupus nephritis is a frequent manifestation in childhood-onset systemic lupus erythematosus (cSLE) and has a great potential for chronic kidney disease (CKD), requiring dialysis and kidney transplantation, with great loss in health-related quality of life. The objective of this study was to analyze renal outcomes and CKD in cSLE and to assess its association with cumulative clinical and laboratory features, current disease activity and damage, cumulative treatments, and outcomes.
Methods: This is a multicenter, nationwide observational study of a cohort of 1,528 cSLE patients followed in 27 Brazilian pediatric rheumatology tertiary centers. All patients fulfilled the American College of Rheumatology (ACR) 1997 criteria for classification of SLE, with disease onset before 18 years of age. In this study, we investigated cumulative risk factors for KF in a large sample of cSLE patients.
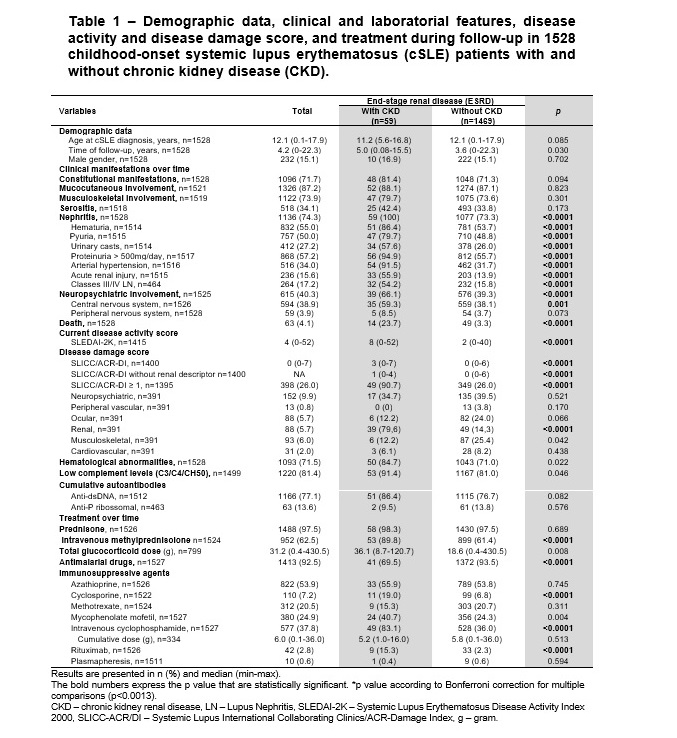
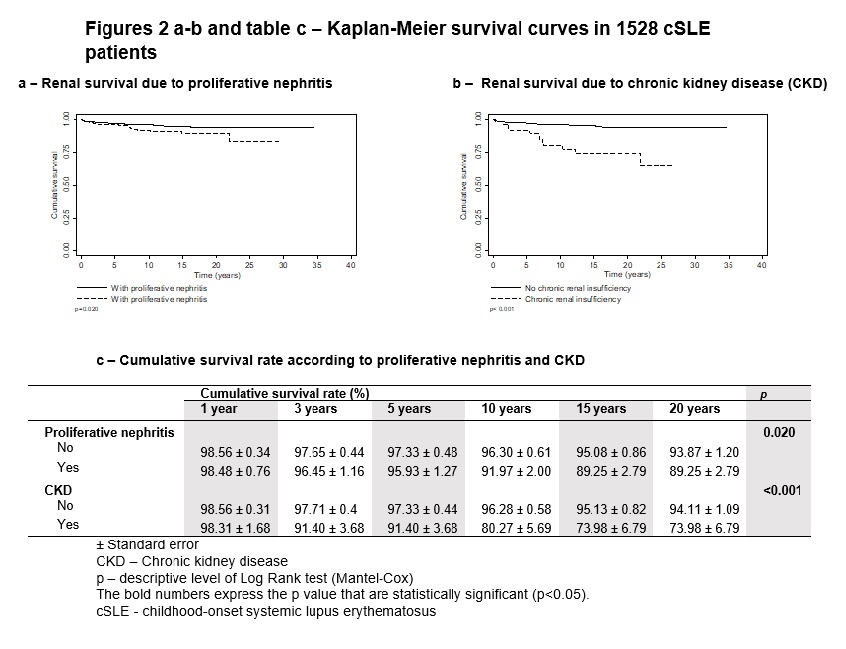
Results: A total of 59/1528 (3.9%) of patients presented CKD. After Bonferroni´s correction for multiple comparisons (p˂0.0013), determinants significantly associated with CKD were urinary sediment alterations, neuropsychiatric involvement, higher scores of current SLEDAI-2K and SLICC/ACR-DI (especially renal involvement), as well as cumulative use of intravenous methylprednisolone, cyclophosphamide, and rituximab. In regression models, arterial hypertension (HR=15.42, 95%CI=6.12-38.83, p≤0.0001) and biopsy-proven proliferative nephritis (HR=2.83, 95%CI=1.70-4.72, p≤0.0001) increased the risk of CKD. The Kaplan-Meier overall curves showed significantly worse patient survival in cSLE patients with biopsy-proven proliferative nephritis (p=0.02) and CKD (p≤0.0001).
Conclusion: This study showed that cSLE patients with arterial hypertension and biopsy-proven proliferative nephritis exhibited higher hazard rates of progression to poor outcomes. Therefore, those patients could benefit from strict blood pressure control during follow-up, and better drug treatment for aggressive management of active lupus nephritis.
To cite this abstract in AMA style:
Sakamoto A, Silva C, Islabão A, Novak G, Molinari B, Pereira R, Saad-Magalhães C, Clemente G, Pioto D, Aikawa N, Pita A, Trindade V, Appenzeller S, Carvalho L, Rabelo-Junior C, Fonseca A, Sztajnbok F, Santos M, Elena Rios Gomes Bica B, Sena E, Moraes A, Fraga M, Robazzi T, Spelling P, Scheibel I, Cavalcanti A, Matos E, Guimarães L, Santos F, Mota L, Bonfá E, Terreri M. Renal Outcomes in 1528 Childhood-onset Systemic Lupus Erythematosus Patients: A Brazilian Multicenter Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/renal-outcomes-in-1528-childhood-onset-systemic-lupus-erythematosus-patients-a-brazilian-multicenter-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-outcomes-in-1528-childhood-onset-systemic-lupus-erythematosus-patients-a-brazilian-multicenter-study/